Generic Drugs: What They Are, How They Save Money, and When to Watch Out
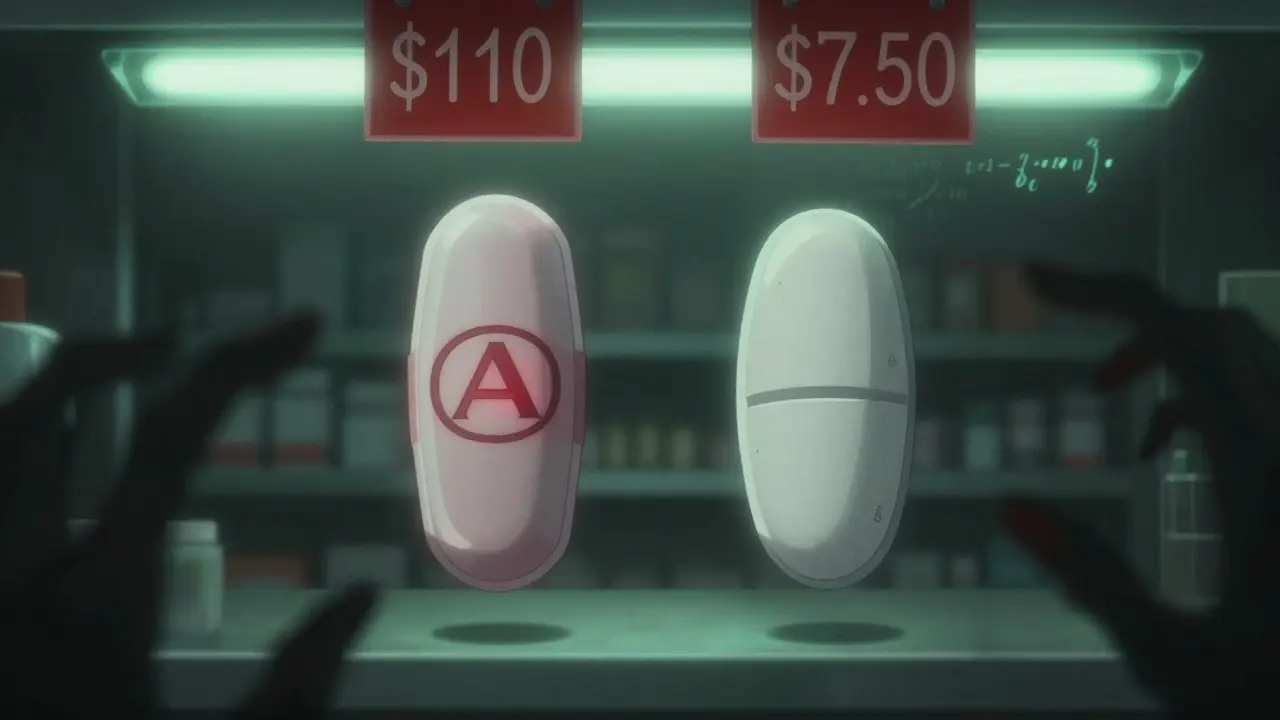
When you hear generic drugs, lower-cost versions of brand-name medications that contain the same active ingredients and meet the same FDA standards. Also known as generic medications, they make up over 90% of prescriptions filled in the U.S. because they work just like the brand-name versions—but cost a fraction of the price. That’s not magic. It’s science and competition. Once a brand-name drug’s patent expires, other companies can make the same pill. The FDA requires these generics to have the same strength, dosage, and effectiveness. No shortcuts. No guesswork. Just the same medicine, cheaper.
But here’s what most people don’t realize: generic drug competition, the market dynamic where multiple manufacturers enter the market and drive prices down through pricing pressure is what makes generics so affordable. When five companies start making the same pill, the price can drop 97%. Medicare and insurers use this competition to negotiate better deals. But sometimes, brands fight back with tricks like "product hopping"—slightly changing the drug just before the patent ends—or paying generic makers to delay their entry. These "reverse payments" aren’t about saving money—they’re about protecting profits.
Then there’s biosimilars, generic versions of complex biologic drugs made from living cells, not chemicals. These aren’t simple pills. They’re injectables like Humira or Enbrel. Biosimilars can cut costs by half, yet most patients don’t even know they exist. Why? Because doctors don’t always suggest them, and pharmacies don’t always stock them. But if you’re on a biologic, asking for a biosimilar could save you thousands a year.
Not all generics are equal, though. For drugs with a narrow therapeutic index, medications where small changes in dosage can cause serious side effects or treatment failure—like warfarin, lithium, or thyroid meds—switching between generic brands can sometimes cause problems. That’s why pharmacists are trained to flag risky switches. The FDA’s CGMP guidelines, Current Good Manufacturing Practices that ensure every batch of generic drug meets strict quality standards are tough, but enforcement isn’t perfect. Some foreign factories cut corners. That’s why verifying drug authenticity matters.
And it’s not just about price. It’s about trust. You take your meds because you need them to work. You shouldn’t have to wonder if your generic is safe, effective, or just cheap. That’s why the posts below cover everything: how to spot overpriced generics, why biosimilars are your secret weapon, how the FDA inspects factories overseas, and when your pharmacist should step in. You’ll find real stories about people who saved hundreds—or lost health—because of a switch they didn’t understand. This isn’t theory. It’s what’s happening in your medicine cabinet right now.
- Jan 29, 2026
- SkyCaddie Fixer
- 8 Comments
Out-of-Pocket Costs: How Generics Cut Your Medication Bills by Up to 95%
Generic drugs save patients up to 95% on medication costs, yet most still overpay due to opaque pricing. Learn how to cut your out-of-pocket expenses with simple, proven strategies.

- Dec 6, 2025
- SkyCaddie Fixer
- 8 Comments
Why Patients Stick to Brand-Name Medications Despite Higher Costs
Despite generics making up 90% of prescriptions, many patients still prefer brand-name medications. This article explores why trust, perception, and emotional safety outweigh cost savings-and what can be done about it.
