Macrolides: What They Are, How They Work, and What You Need to Know
When your doctor prescribes an antibiotic for a stubborn sinus infection, bronchitis, or strep throat, they might reach for a macrolide, a class of antibiotics that block bacteria from making proteins they need to survive. Also known as macrocyclic lactones, these drugs have been around since the 1950s and still play a vital role in treating common infections today.
Macrolides like azithromycin, a once-daily antibiotic often used for pneumonia and chlamydia, and clarithromycin, commonly paired with other drugs to treat stomach ulcers caused by H. pylori, are favorites because they’re well-tolerated and work against a broad range of bacteria. erythromycin, the original macrolide, is still used when patients can’t take penicillin. These drugs don’t just kill bacteria—they slow them down enough for your immune system to catch up. That’s why they’re often chosen for lung infections where fast-acting drugs might cause too much inflammation.
But here’s the catch: overuse has made some bacteria resistant. If you’ve ever taken azithromycin for a sore throat and it didn’t help, that’s likely why. Macrolide resistance is rising fast, especially in places where antibiotics are handed out too easily. That’s why doctors now avoid them for viral colds and mild infections. They’re not magic pills—they’re targeted tools. And using them wrong makes them useless for everyone.
What you won’t find in most patient brochures is how macrolides interact with other meds. They can mess with heart rhythm if you’re on certain statins or antiarrhythmics. They can boost the effect of blood thinners, making bleeding more likely. Even some herbal supplements like St. John’s wort can reduce their power. That’s why knowing what else you’re taking matters just as much as knowing the name of the drug.
There’s also a surprising side effect: macrolides aren’t just antibiotics. Low-dose, long-term use of azithromycin is sometimes prescribed for chronic lung diseases like bronchiectasis or COPD—not to kill bacteria, but to reduce inflammation. It’s a different use, but it’s real, and it’s backed by clinical studies. This isn’t theory—it’s practice.
What you’ll find in the posts below are real, no-fluff guides on how macrolides fit into everyday health. You’ll see how they compare to other antibiotics, what side effects actually happen, how to spot when they’re being overused, and why some people respond better than others. No jargon. No marketing. Just what you need to know to ask the right questions and stay safe.
- Dec 1, 2025
- SkyCaddie Fixer
- 11 Comments
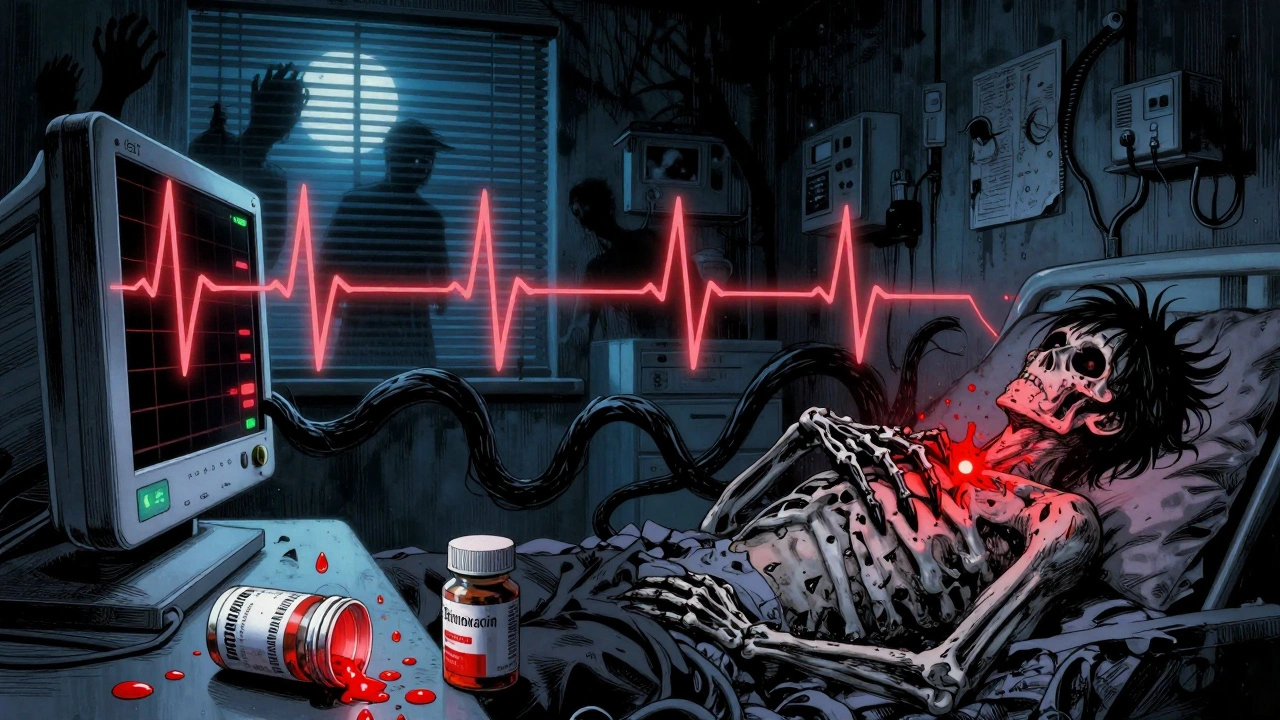
QT Prolongation with Fluoroquinolones and Macrolides: What Doctors Need to Monitor
Fluoroquinolones and macrolides can prolong the QT interval, raising the risk of life-threatening heart rhythms. Learn who needs ECG monitoring, which antibiotics are safest, and how to prevent fatal arrhythmias.
