When you’re prescribed Tinidazole for an infection like trichomoniasis or bacterial vaginosis, you might wonder: is this the best option? Or are there other pills out there that work just as well-or better? You’re not alone. Many people ask the same thing after reading the side effects or hearing about other drugs from friends or online forums. The truth is, Tinidazole isn’t the only choice. But how do you know which alternative is right for you?
What Tinidazole Actually Does
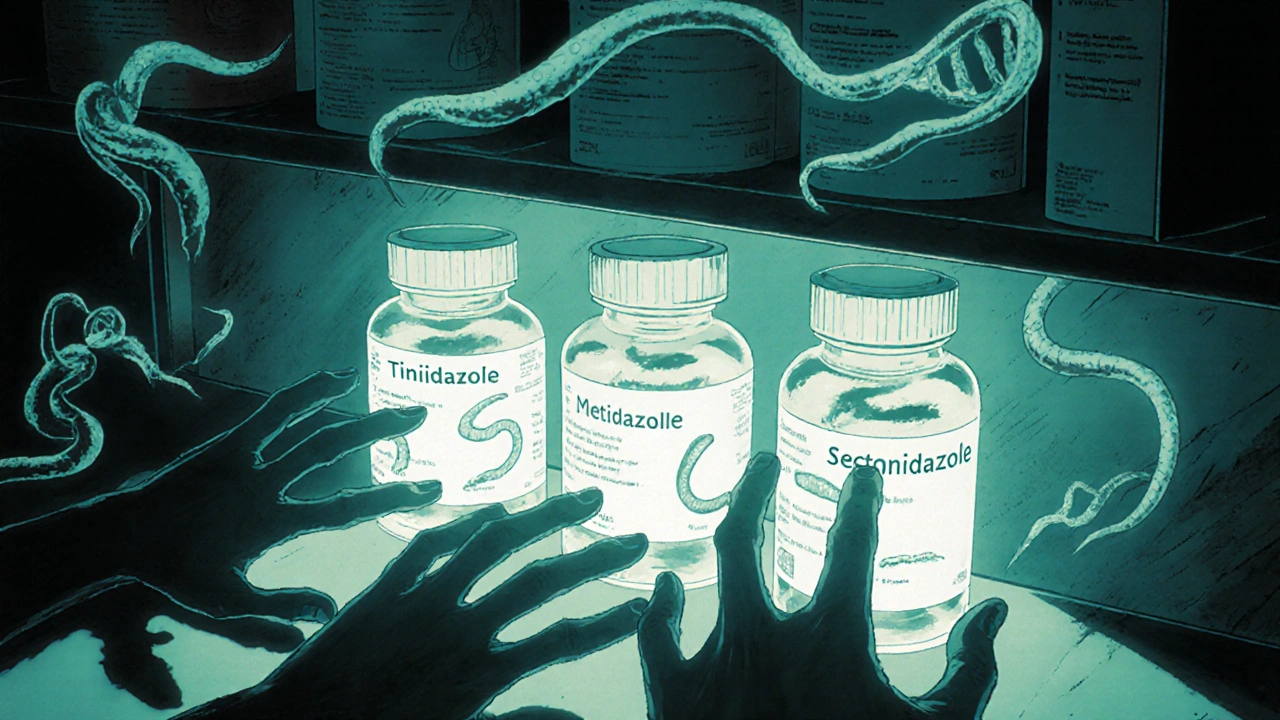
Tinidazole is an antibiotic and antiprotozoal medication used to treat infections caused by anaerobic bacteria and certain parasites. It was first approved in the 1970s and belongs to the nitroimidazole class of drugs, the same group as metronidazole. It kills organisms like Trichomonas vaginalis, Giardia lamblia, and Bacteroides species by damaging their DNA.
Doctors often prescribe it as a single 2-gram dose for trichomoniasis, or a 500mg dose twice daily for 5-7 days for bacterial vaginosis. Compared to older treatments, Tinidazole has a longer half-life-about 12-14 hours-meaning you take fewer pills. That’s one reason it’s popular: convenience.
But it’s not perfect. Side effects include nausea, a metallic taste in the mouth, dizziness, and headaches. And if you drink alcohol while taking it, you’ll get a severe reaction: vomiting, rapid heartbeat, flushing. That’s true for all nitroimidazoles.
Metronidazole: The Original Alternative
Metronidazole is the most common alternative to Tinidazole and has been used since the 1960s. It’s the drug Tinidazole was designed to improve upon.
For trichomoniasis, metronidazole is usually given as 500mg twice daily for 7 days. For bacterial vaginosis, it’s the same dosing or a single 2-gram dose. It works the same way as Tinidazole-damaging parasite and bacterial DNA.
So why use one over the other? Here’s the real difference: Tinidazole stays in your system longer, so you take fewer doses. Metronidazole is cheaper and more widely available, especially in public health clinics. But it’s more likely to cause stomach upset. A 2021 study in the Journal of Antimicrobial Chemotherapy found that 38% of patients on metronidazole reported nausea, compared to 22% on Tinidazole.
Also, metronidazole comes in more forms: tablets, gel, and even vaginal suppositories. That gives doctors more options for treating localized infections.
Secnidazole: The Once-Daily Option
Secnidazole is a newer nitroimidazole, approved in the U.S. in 2018, and designed specifically for single-dose treatment.
For trichomoniasis and bacterial vaginosis, you take one 2-gram tablet. That’s it. No second dose. No 5-day course. Just one pill. That’s the big selling point.
It has the same side effects as Tinidazole and metronidazole-nausea, headache, metallic taste-but because it’s a single dose, many people find it easier to tolerate. A 2023 clinical trial published in Obstetrics & Gynecology showed that 89% of patients completed secnidazole treatment without stopping due to side effects, compared to 81% for metronidazole.
Downside? It’s expensive. In Australia, a single 2-gram tablet can cost over $120 without a subsidy. In the U.S., it’s covered by many insurance plans, but out-of-pocket costs are still high. Tinidazole and metronidazole are often under $10 with a prescription.

Other Alternatives: Are There Any?
There aren’t many true alternatives outside the nitroimidazole family. That’s because these drugs target anaerobic organisms in a very specific way. Other antibiotics like doxycycline or azithromycin won’t work for trichomoniasis or bacterial vaginosis.
Some people try natural remedies-probiotics, garlic, tea tree oil. But there’s no strong evidence they cure these infections. The CDC and WHO don’t recommend them as replacements for antibiotics. If you’re trying to avoid medication, you risk the infection spreading or coming back worse.
One exception: for recurrent bacterial vaginosis, some doctors add boric acid suppositories after antibiotic treatment. It helps rebalance vaginal pH and reduces recurrence rates by up to 60% in some studies. But it’s not a replacement for Tinidazole-it’s a follow-up tool.
Which One Should You Choose?
Let’s cut through the noise. Here’s a simple decision guide based on real-world use:
- Choose Tinidazole if you want fewer doses than metronidazole but need something cheaper than secnidazole. Good balance of effectiveness, cost, and convenience.
- Choose Metronidazole if cost is your biggest concern and you can stick to a 5-7 day schedule. It’s the most tested and widely available.
- Choose Secnidazole if you hate taking pills daily and can afford it. Best for people who struggle with adherence.
Also consider your lifestyle. If you’re traveling, going out of town, or don’t want to remember to take pills for a week, the single-dose option (secnidazole or Tinidazole) makes sense. If you’re on a tight budget or your clinic only stocks metronidazole, that’s still a perfectly valid choice.
What About Alcohol?
Yes, you need to avoid alcohol with all of these drugs. It’s not a myth. Even a small amount-like a glass of wine or a beer-can trigger a reaction within minutes. Symptoms include:
- Severe nausea and vomiting
- Flushing and rapid heartbeat
- Headache and dizziness
- Low blood pressure
That reaction happens because these drugs block the enzyme that breaks down alcohol in your liver. The buildup of acetaldehyde causes the symptoms. It’s not dangerous for most people, but it’s extremely unpleasant.
Doctors recommend avoiding alcohol for at least 72 hours after your last dose. Some people wait a full week to be safe. If you’re unsure, ask your pharmacist. They’ll know your exact medication and dosage.

What If It Doesn’t Work?
Failure rates for all three drugs are low-under 10% for trichomoniasis when taken correctly. But if symptoms come back, it’s not always because the drug failed.
Common reasons treatment doesn’t work:
- You didn’t take the full dose
- Your partner wasn’t treated (trichomoniasis is sexually transmitted)
- You drank alcohol during treatment
- The strain is resistant (rare, but possible)
If you’re still symptomatic after finishing the course, go back to your doctor. They may switch you to a longer course of metronidazole (7-10 days) or try a different approach. Resistance to nitroimidazoles is still very uncommon, so don’t assume it’s the drug’s fault.
Final Thoughts
Tinidazole isn’t the best for everyone. But it’s not the worst, either. It’s a middle ground-effective, convenient, and affordable. Metronidazole is the workhorse. Secnidazole is the premium option. The right choice depends on your budget, lifestyle, and how well you can stick to a schedule.
Don’t let fear of side effects stop you from treating the infection. Untreated trichomoniasis can increase your risk of HIV transmission. Bacterial vaginosis can lead to pelvic inflammatory disease or complications during pregnancy. These drugs work. You just need to pick the one that fits your life.
Can I take Tinidazole if I’m pregnant?
Yes, Tinidazole is considered safe during pregnancy, especially after the first trimester. The CDC lists it as an option for treating trichomoniasis in pregnant women. However, your doctor will weigh the risks and benefits. Metronidazole is more commonly used in pregnancy because it’s been studied longer. Always consult your OB-GYN before taking any antibiotic while pregnant.
Is Tinidazole better than metronidazole for bacterial vaginosis?
Tinidazole is slightly more effective and better tolerated than metronidazole for bacterial vaginosis. A 2020 Cochrane review found that cure rates were similar-around 85%-but side effects were lower with Tinidazole. The main advantage is convenience: a single 2-gram dose vs. 5-7 days of pills. If you can get it at a reasonable price, Tinidazole is often the preferred choice.
How long does Tinidazole stay in your system?
Tinidazole has a half-life of about 12-14 hours, meaning it takes roughly 3 days for your body to clear most of it. For safety, avoid alcohol for at least 72 hours after your last dose. If you’re taking it for 5 days, wait a full week before drinking. This reduces the risk of any delayed reaction.
Can I buy Tinidazole over the counter?
No. Tinidazole is a prescription-only medication in Australia, the U.S., and most other countries. You cannot buy it legally without a doctor’s prescription. Online pharmacies selling it without a prescription are unregulated and often sell fake or contaminated products. Always get it from a licensed pharmacy with a valid prescription.
Do I need to treat my partner if I have trichomoniasis?
Yes. Trichomoniasis is a sexually transmitted infection. If your partner isn’t treated, you’ll likely get reinfected-even if you took the medication perfectly. Both partners should be treated at the same time, even if one has no symptoms. Avoid sex until both of you have finished treatment and symptoms are gone.
What to Do Next
If you’ve been prescribed Tinidazole and are unsure whether it’s right for you, talk to your pharmacist. They can tell you about cost, availability, and whether secnidazole or metronidazole might be a better fit. If you’re dealing with recurring infections, ask about follow-up care-like probiotics or pH-balancing treatments.
Don’t delay treatment. These infections don’t go away on their own. And while the side effects of Tinidazole can be annoying, they’re temporary. The consequences of leaving them untreated? Not worth the risk.

Ankit Yadav
November 5, 2025 AT 10:56Tinidazole saved my ass when metronidazole gave me nausea so bad I thought I was dying. Single dose? Yes please. I took it while traveling and didn’t have to carry pills around for a week. Alcohol? I waited 10 days just to be safe. Worth it.
Meghan Rose
November 5, 2025 AT 13:48I tried secnidazole last year and it was like magic-one pill and done. But holy hell was it expensive. My insurance covered it but I paid $80 out of pocket. Worth it? Maybe. Would I do it again? Only if I was too lazy to take pills for a week.
Steve Phillips
November 6, 2025 AT 07:21Let’s be real-Tinidazole isn’t ‘better’ than metronidazole, it’s just the pharmaceutical industry’s rebranding of the same damn drug with a 300% markup. Metronidazole has been around since Nixon was president and still kicks ass. Secnidazole? That’s just a fancy pill for people who think ‘convenience’ is a medical condition. Also-alcohol warning? Please. I’ve had wine after metronidazole and lived to tell the tale. Your body isn’t a nuclear reactor.
Rachel Puno
November 6, 2025 AT 19:41For anyone scared of side effects-just know this: untreated infections are way worse. I had recurrent BV for years and was terrified of antibiotics. Then I tried Tinidazole-single dose, no drama, and my life changed. Don’t let fear stop you. Talk to your doc. Ask about probiotics afterward. You got this.
Clyde Verdin Jr
November 8, 2025 AT 02:06Y’all are acting like this is a Netflix documentary. It’s a damn antibiotic. One pill, one side effect, one alcohol warning. And now someone’s gonna say ‘I used garlic’ and ruin the thread. 😭🫠
Key Davis
November 9, 2025 AT 18:07As a healthcare professional with over two decades of clinical experience, I must emphasize that while pharmacokinetic advantages exist with Tinidazole and Secnidazole, the foundational efficacy of Metronidazole remains unparalleled in public health contexts. Cost accessibility, global supply chain reliability, and documented long-term safety profiles render it the most responsible first-line agent in resource-constrained environments. The notion of ‘premium’ alternatives must be weighed against equitable access.
Cris Ceceris
November 9, 2025 AT 20:18It’s wild how we treat antibiotics like they’re all the same, but each one carries a whole history-metronidazole from the 60s, tinidazole as the quieter cousin who showed up late but stayed longer, secnidazole the overachiever who just wants to be done with it all. And yet, we’re still just trying to kill microscopic organisms that don’t even care if we’re tired or broke. Makes you wonder how we got this far.
Brad Seymour
November 10, 2025 AT 16:53My partner and I both got treated at the same time after I found out I had trichomoniasis. We didn’t even argue about it. Just got the scripts, avoided booze for a week, and moved on. No drama. Just responsibility. If you’re reading this and thinking ‘I’ll just wait,’ trust me-it’s not worth it. Get treated. Get your partner treated. Life’s too short for repeat infections.