nausea management
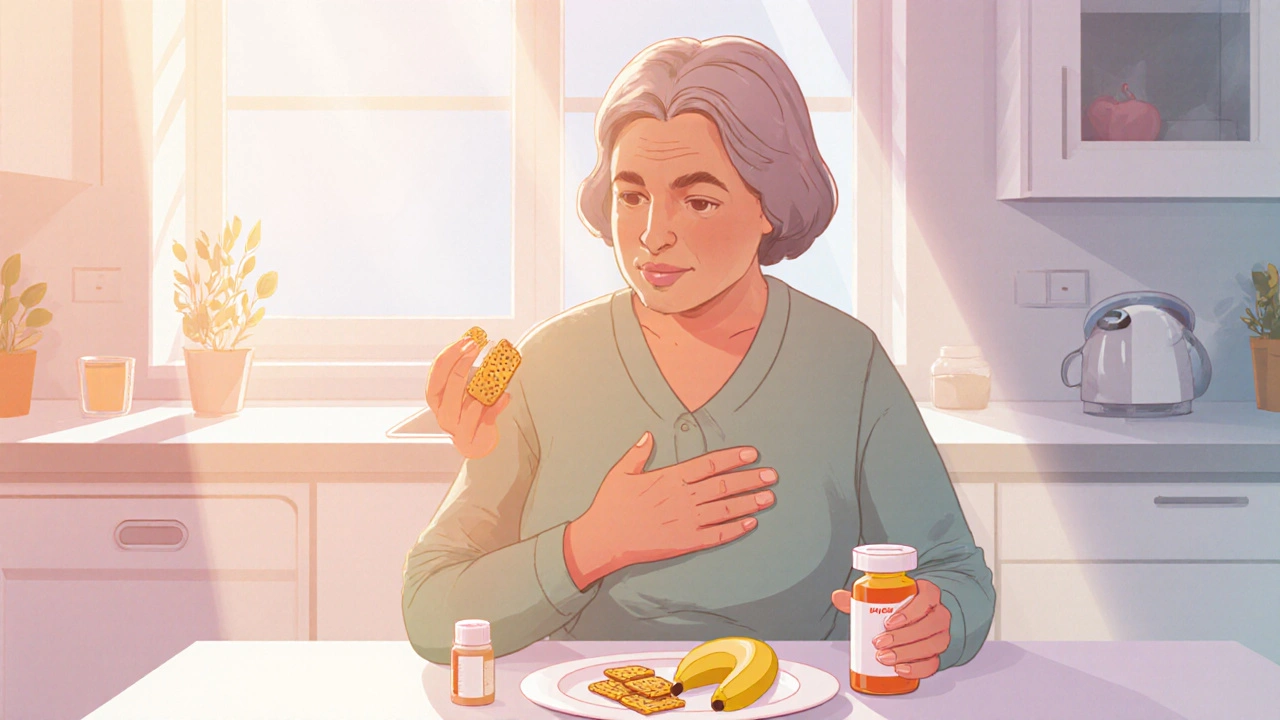
When dealing with nausea management, the practice of reducing or preventing the uncomfortable feeling of nausea through diet, medication, and lifestyle tweaks. Also known as anti‑nausea care, it helps people stay comfortable during illness, treatment, or travel.
Effective antiemetic therapy, the use of drugs that block nausea signals in the brain and gut is a core pillar of nausea management. These medicines, like ondansetron or metoclopramide, work quickly but often require strict medication adherence, following the prescribed schedule and dosage without missing doses to keep symptoms at bay. Missing a dose can let nausea flare up again, especially when the body is already stressed by illness or chemotherapy.
Beyond pills, dietary adjustments, changes in what and how you eat to calm the stomach play a surprisingly big role. Small, bland meals, ginger tea, and avoiding strong odors help keep the stomach settled. Eating slowly and sipping water between bites also reduces the chance of an upset. This approach aligns with the idea that "nausea management includes dietary adjustments" – a simple but powerful semantic connection.
Staying well‑hydrated is another often‑overlooked tactic. hydration, regular intake of fluids like water, electrolyte drinks, or clear broths can dilute stomach acids and support overall digestive health. Dehydration often worsens nausea, so sipping fluids throughout the day can blunt the symptom’s intensity. In practice, "effective nausea management requires adequate hydration" forms a clear link between fluid intake and symptom control.
When nausea stems from medication side effects, a combined strategy works best. Talk to a healthcare provider about switching to a less upsetting drug or adding a low‑dose antiemetic. Pair that with the dietary and hydration tips above, and you create a multi‑layered defense. This mirrors the semantic triple: "nausea management combines antiemetic therapy, dietary adjustments, and hydration to reduce symptoms."
Stress and anxiety can also trigger nausea, especially during travel or exams. Simple relaxation techniques—deep breathing, short walks, or guided meditation—help calm the nervous system. Think of these practices as an auxiliary tool that supports the primary pillars of medication, diet, and fluids. By acknowledging the mind‑body link, you broaden the scope of nausea management beyond just pills and food.
Below you’ll find a curated set of articles that dive deeper into each of these areas. From detailed guides on antiemetic medication adherence to practical tips on ginger‑based dietary tricks, the collection covers the full spectrum of nausea management. Whether you’re coping with treatment‑related nausea or occasional stomach upset, the resources will give you actionable steps you can try right away.
Take a look at the posts ahead to learn how specific treatments, lifestyle tweaks, and supportive habits come together to keep nausea in check. Each piece adds a piece to the puzzle, helping you build a personalized plan that fits your routine and health needs.
- Oct 16, 2025
- SkyCaddie Fixer
- 10 Comments
How to Manage Nausea While Taking Conjugated Estrogens USP
Learn practical steps to curb nausea caused by Conjugated Estrogens USP, from diet tweaks and OTC remedies to when you should see a doctor.
