Hormone Therapy Side Effects
When dealing with hormone therapy side effects, the unwanted physical and mental changes that can arise from using hormones to treat medical conditions. Also known as hormone replacement therapy adverse effects, they can impact anyone on hormone regimens. The risk profile shifts when you add Estrogen therapy, a treatment often prescribed for menopausal symptoms or low estrogen levels, Testosterone replacement, supplementation aimed at men with low testosterone or women with specific endocrine disorders, or even short bursts of Corticosteroid therapy, potent anti‑inflammatory drugs used for asthma, arthritis, and autoimmune conditions. Each of these approaches brings its own set of side effects, but they also share common threads: mood swings, weight changes, and cardiovascular strain. Understanding hormone therapy side effects helps you stay ahead of problems, because early detection lets you adjust dosage, add protective measures, or switch to alternatives before complications become serious.
Key Considerations Across Hormone Types
Metabolic shifts are a big part of the picture. Estrogen therapy can raise triglyceride levels and, in rare cases, increase clotting risk, while testosterone replacement may lead to higher red‑blood‑cell counts and potential sleep‑apnea issues. Corticosteroids are notorious for causing blood‑sugar spikes, bone loss, and facial rounding. Beyond metabolism, mood and cognition feel the impact: many patients report anxiety, irritability, or memory fog during the first weeks of treatment. Bone health deserves a mention, too—long‑term estrogen or testosterone use can either protect or weaken bone density depending on dose and patient age. Thyroid hormone therapy, another related entity often grouped with hormone replacement, brings its own challenges such as heart‑rate acceleration or excessive weight loss if over‑treated. Growth hormone therapy, though less common, can cause joint pain and insulin resistance. All these side effects share a common denominator: they require regular monitoring, lab work, and open dialogue with your doctor. By tracking blood work, symptom diaries, and lifestyle changes, you can catch problems early and tweak treatment plans before they snowball.
Practical steps can cut many of these risks. Keep a simple log of any new symptoms—headaches, mood dips, swelling, or changes in sleep patterns. Schedule routine blood tests to watch hormone levels, cholesterol, glucose, and bone markers. Pair medication with a balanced diet rich in calcium, vitamin D, and omega‑3 fatty acids to protect bone and heart health. Exercise, especially weight‑bearing activities, counters steroid‑induced bone loss and helps manage weight changes from estrogen or testosterone. If you notice severe side effects—persistent high blood pressure, sudden weight gain, or deep vein thrombosis—contact your provider immediately. The goal isn’t to scare you but to give you tools to stay in control. Below you’ll find a collection of articles that drill down into each side effect, share management tips, and highlight the latest research so you can make informed choices about your hormone therapy journey.
- Oct 16, 2025
- SkyCaddie Fixer
- 10 Comments
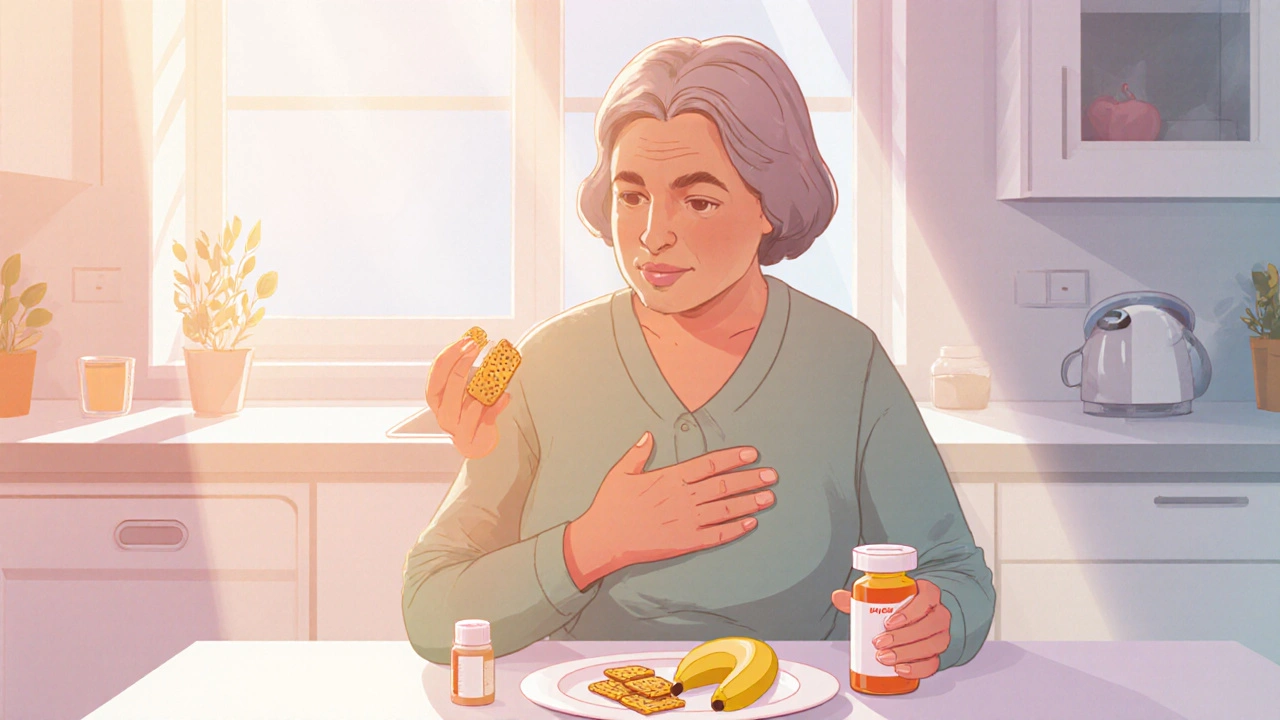
How to Manage Nausea While Taking Conjugated Estrogens USP
Learn practical steps to curb nausea caused by Conjugated Estrogens USP, from diet tweaks and OTC remedies to when you should see a doctor.
