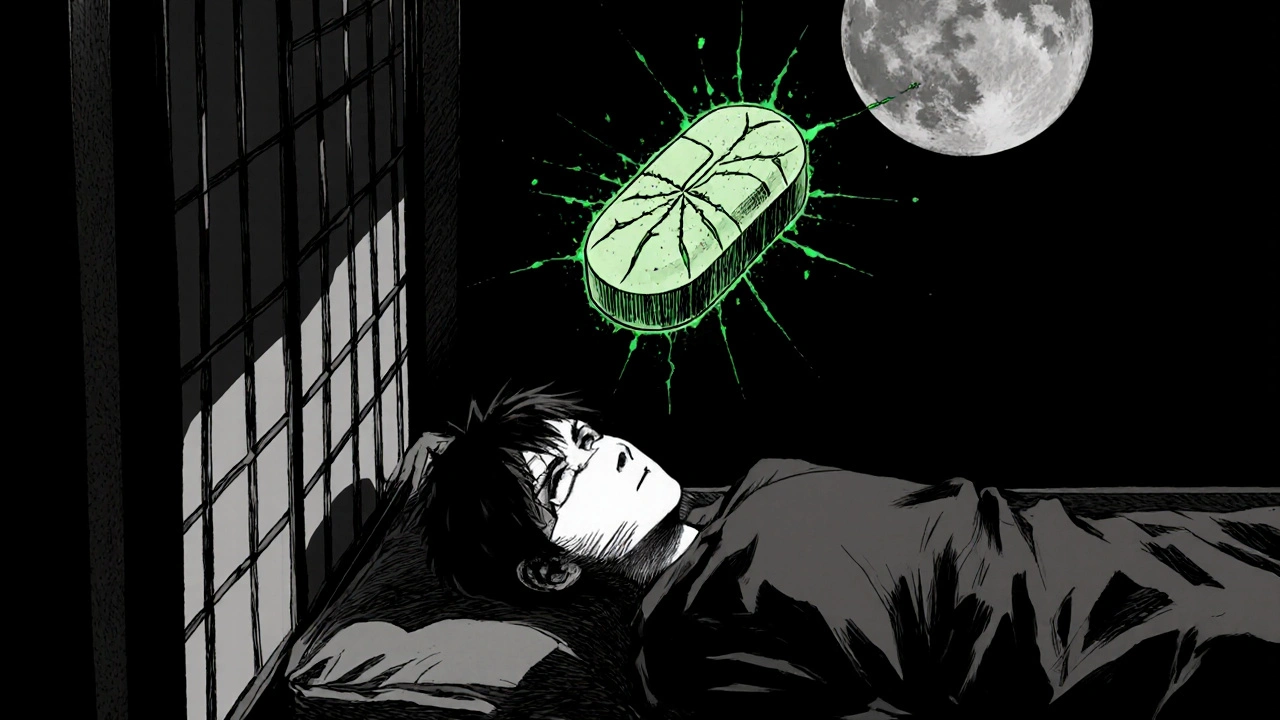
Antiretroviral Insomnia: Causes, Symptoms, and Practical Tips
When dealing with antiretroviral insomnia, a sleep disturbance that shows up while taking antiretroviral medication for HIV. Also known as ART‑related sleep problems, it sits at the crossroads of two other key ideas: antiretroviral therapy and insomnia. Understanding how these pieces fit together helps you spot triggers early and choose the right fixes.
Why Sleep Gets Messed Up While on HIV Meds
Antiretroviral insomnia encompasses three main drivers. First, many drugs in the regimen hit the brain’s neurotransmitters, shifting the balance that normally puts you to sleep. Second, HIV itself can raise inflammatory markers that keep the nervous system on high alert, making it harder to wind down. Third, lifestyle factors—like irregular meals, night‑time caffeine, or stress about the diagnosis—add fuel to the fire. In short, the condition requires a look at both medication side effects and overall sleep hygiene.
Clinical studies show that patients on protease inhibitors report 30‑40 % more night‑time awakenings than those on newer integrase‑strand transfer inhibitors. That statistic tells us the type of antiretroviral therapy matters. Switching to a regimen with a lower central‑nervous‑system impact often reduces the frequency of waking up. At the same time, evaluating the timing of doses—taking a stimulating pill too close to bedtime—can make a big difference.
Another piece of the puzzle is the link between HIV infection and the body’s circadian rhythm. Research from 2023 linked elevated cytokine levels to delayed melatonin release, which explains why many patients feel groggy in the morning even if they slept eight hours. Recognizing this connection influences how you approach treatment: a low‑dose melatonin supplement or a light‑therapy box in the morning can help reset the clock.
Practical Steps to Calm the Night
Managing antiretroviral insomnia starts with a two‑pronged plan: adjust the medication side where possible, and adopt sleep‑friendly habits. Here’s a quick checklist you can try tonight:
- Ask your doctor if a switch to a newer ART class (like integrase inhibitors) is feasible.
- Move the dose of any stimulant‑type med (e.g., efavirenz) to early afternoon.
- Set a regular bedtime and keep the bedroom cool, dark, and quiet.
- Limit caffeine after 2 PM and replace it with herbal tea.
- Practice a 5‑minute breathing or progressive‑muscle‑relaxation routine before lights out.
- If you wake up, avoid checking the phone; instead, focus on slow breathing for a few minutes.
These actions target both the medication side effects and the behavioral factors that keep insomnia in check. For many people, just shifting the pill schedule and adding a short wind‑down ritual reduces nighttime awakenings by half.
When simple tweaks aren’t enough, a short course of a non‑habit‑forming sleep aid (like low‑dose trazodone) can bridge the gap while you work on the underlying causes. Always discuss dosage and duration with your provider—most guidelines recommend no more than four weeks before reassessing.
Below you’ll find a curated list of articles that dig deeper into each of these angles: from the science behind ART‑related sleep changes to real‑world tips for better rest. Dive in to see how the latest research, medication guides, and lifestyle tricks can help you reclaim a full night’s sleep.
- Oct 25, 2025
- SkyCaddie Fixer
- 12 Comments
Disoproxil and Sleep: How the Drug Affects Sleep Quality
Explore how Disoproxil, a key HIV/hepatitis B drug, can affect sleep quality, why it happens, and practical steps to manage insomnia while staying on treatment.
