What Are Steroid Eye Drops and Why Are They Used?
Steroid eye drops, also known as corticosteroid ophthalmic solutions, are powerful medications designed to calm down inflammation in the eye. Common brands include Pred Forte, a brand of prednisolone acetate used to treat severe eye inflammation, Omnipred, a weaker formulation of prednisolone for milder cases, and dexamethasone, a potent steroid often used for uveitis or post-surgical swelling. These drops work by blocking the body’s inflammatory response at the cellular level-slowing down chemicals like prostaglandins and phospholipase A2 that cause redness, swelling, and pain.
They’re not for every eye problem. You won’t use them for a simple cold or viral pink eye. But if you have uveitis, inflammation of the middle layer of the eye that can threaten vision, allergic conjunctivitis, chronic eye allergies with swelling and itching, or damage from a chemical splash or burn, steroid drops can be lifesaving. Many patients see improvement within days. For someone with acute uveitis, these drops can mean the difference between keeping their vision and losing it.
The Real Benefits: Fast Relief When It Matters Most
The biggest advantage of steroid eye drops is how quickly they work. Unlike antibiotics, which fight bacteria, or antihistamines, which only ease allergy symptoms, steroids target the root cause of inflammation. This makes them uniquely effective for conditions where swelling is the main threat.
Take uveitis, for example. Left untreated, it can cause permanent scarring in the iris, lead to glaucoma, or even cause the retina to detach. In a 2017 case review by the American Optometric Association, over 80% of patients with non-infectious uveitis showed major improvement within two weeks of starting prednisolone drops. Dr. Daniel Bintz, an optometrist with decades of experience, noted that most patients respond well-so long as the drops are used correctly and stopped on time.
For people recovering from eye surgery, like cataract removal, these drops help prevent the eye from reacting too strongly to the procedure. Without them, scar tissue could form, clouding vision even after a successful operation. In cases of severe allergic reactions-like those triggered by pollen, pet dander, or even makeup-steroid drops can stop the cycle of swelling that makes eyes feel like they’re on fire.
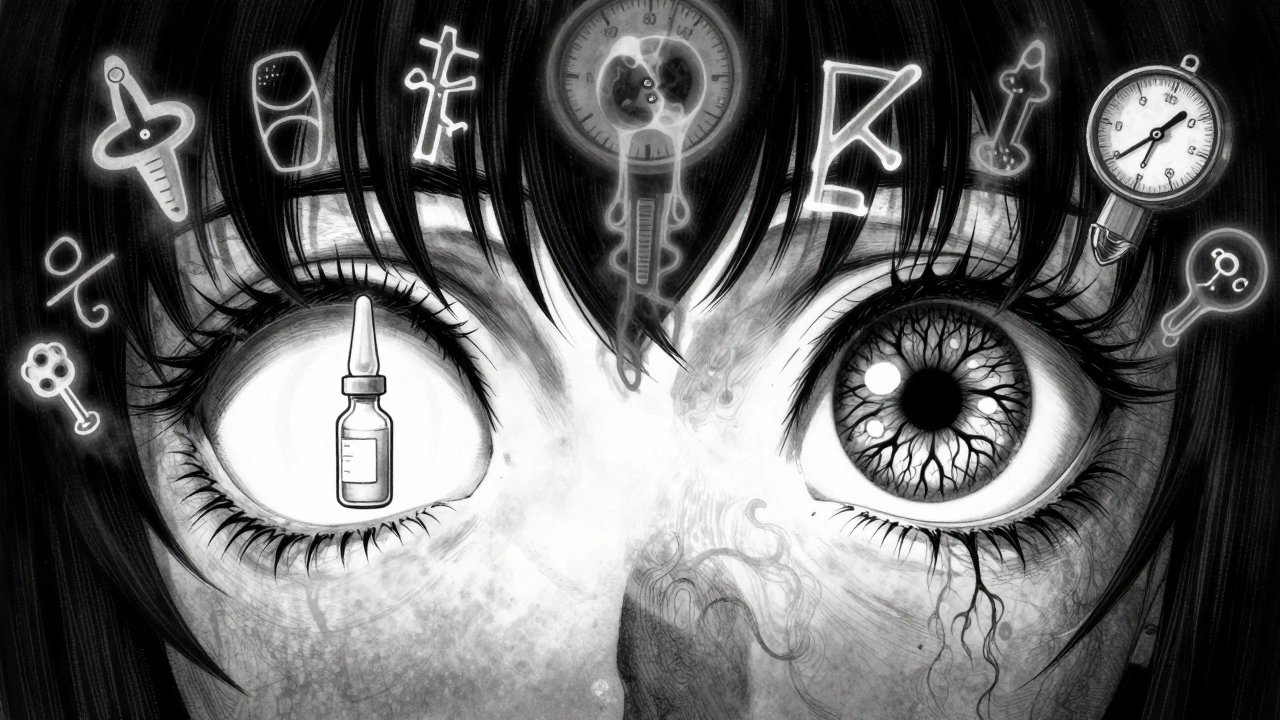
The Hidden Dangers: Steroid-Induced Glaucoma and Cataracts
Here’s the catch: these powerful drops come with serious risks if used too long or without monitoring. The two biggest dangers are steroid-induced glaucoma, a type of pressure-related optic nerve damage caused by corticosteroids and posterior subcapsular cataracts, a clouding of the lens that forms at the back and blocks central vision.
Glaucoma from steroids doesn’t always cause pain or obvious symptoms. In fact, most people don’t feel anything until their vision is already damaged. About 30-40% of people will see a small rise in eye pressure when using these drops. But 4-6% are "steroid responders"-their pressure spikes dangerously high, sometimes over 30 mmHg. That’s like having your eye under constant stress. Over weeks or months, this pressure crushes the optic nerve, leading to blind spots, tunnel vision, and eventually, irreversible blindness.
Cataracts are another silent threat. While age-related cataracts develop slowly over decades, steroid use can accelerate the process. Studies show that using potent drops like prednisolone acetate for more than 10 days increases the risk. After three to six months, the chance of developing a cataract becomes significant. These aren’t the typical cloudy lenses you see in older adults-they form right in the center of the lens, directly in your line of sight. That means blurry vision, glare from lights, and trouble reading even when your eye pressure is normal.
Who’s at Highest Risk?
Not everyone reacts the same way to steroid eye drops. Certain people are far more likely to develop complications. If you have any of these, your doctor should be extra cautious:
- Pre-existing glaucoma-even if it’s controlled, steroids can push pressure back up.
- Family history of glaucoma-genetics play a big role in how your eyes respond.
- Diabetes-high blood sugar already stresses the eye’s blood vessels; steroids add more strain.
- Previous cataract surgery-your eye is more sensitive to inflammation and pressure changes.
- Long-term steroid use-anything beyond 4 weeks significantly raises risk.
Even if you’re young and healthy, if you’re using high-dose drops for more than two weeks, you’re in the danger zone. The American Academy of Ophthalmology says that anyone on steroids for over 10 days needs regular pressure checks. Don’t assume you’re fine just because you don’t feel pain.
How to Monitor Your Eyes Safely
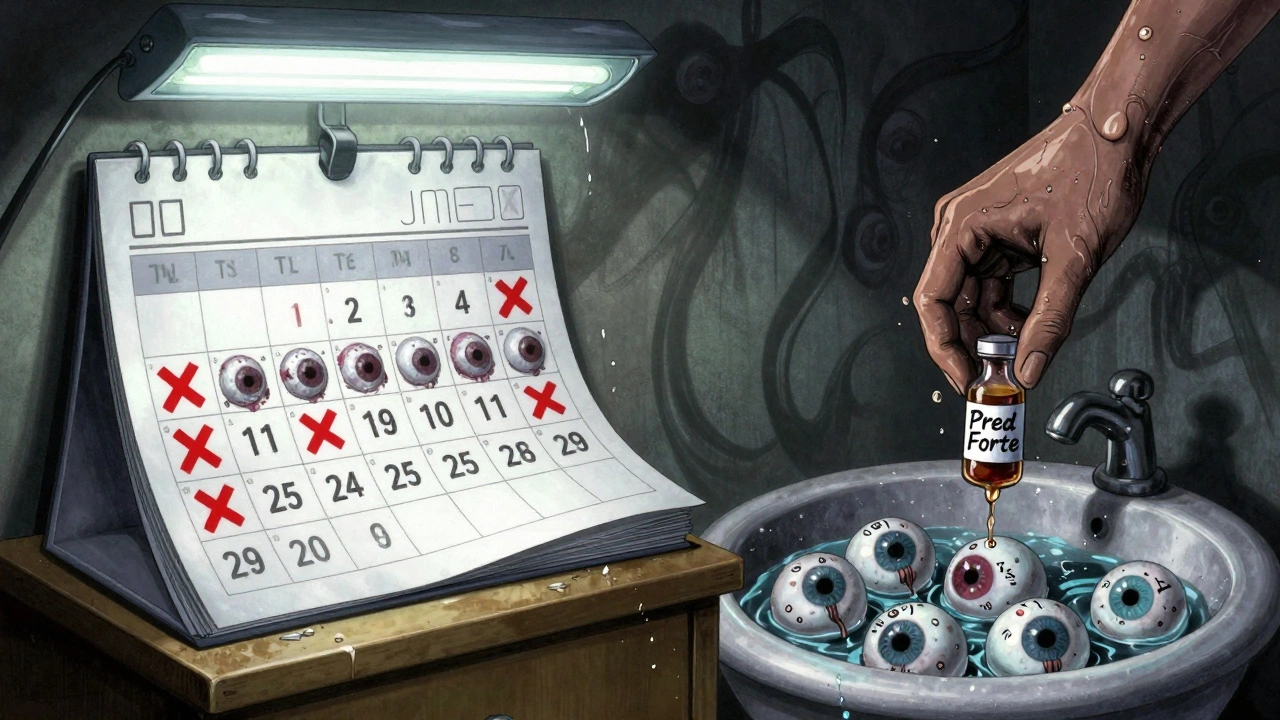
Monitoring isn’t optional-it’s mandatory. If your doctor prescribes steroid drops for more than 10 days, you need scheduled eye exams. Here’s what that looks like:
- Baseline exam before starting-your eye pressure is measured with Goldmann applanation tonometry (the gold standard), your optic nerve is checked, and your lens is examined for early clouding.
- First follow-up: 2-4 weeks after starting-if you’re on a low dose or have no risk factors, this is enough. If you’re on a high-potency drop like Pred Forte, or have diabetes or glaucoma, you’ll need to come back every 1-2 weeks.
- Every 4 weeks during treatment-pressure checks continue. Your doctor will also look for signs of infection, corneal thinning, or early cataract formation.
- After stopping-pressure can stay high for weeks after you stop the drops. A final check at 4-6 weeks ensures your eye has returned to normal.
Don’t skip these visits. Many people think, "I feel fine," but by the time they notice blurry vision or peripheral blind spots, the damage is done. Glaucoma doesn’t hurt until it’s too late. That’s why regular pressure checks are the only way to catch it early.
When to Stop-and How to Do It Right
Steroid eye drops aren’t meant for long-term use. Most inflammatory eye conditions improve within 2-8 weeks. After that, the risks outweigh the benefits. Your doctor will usually taper the dose instead of stopping cold turkey. Why? Stopping suddenly can cause rebound inflammation-your eye can flare up worse than before.
For example, if you were using Pred Forte four times a day, your doctor might reduce it to three times a day for a week, then twice a day for another week, then once daily for a few days before stopping. This slow withdrawal gives your eye time to heal without triggering a flare-up.
If you’ve been on drops for more than a month, your doctor may switch you to a non-steroidal anti-inflammatory (NSAID) eye drop like ketorolac. These don’t carry the same glaucoma or cataract risks. They’re weaker, but safer for ongoing use. Some patients with chronic allergies or mild uveitis can manage long-term with NSAIDs alone.
Symptoms That Mean You Need to Call Your Doctor Immediately
Even with monitoring, complications can sneak up. If you notice any of these, don’t wait for your next appointment:
- Blurry vision that doesn’t improve
- Eye pain or a feeling of pressure behind the eye
- Seeing halos around lights or increased glare at night
- Loss of side vision (tunnel vision)
- Redness that gets worse instead of better
- Eye discharge or a feeling like something’s stuck in your eye
These could mean rising pressure, a new cataract, or even a serious infection like fungal keratitis. Steroids suppress your eye’s immune system, so even a tiny scratch can turn into a sight-threatening infection. Don’t ignore these signs.
Alternatives and Long-Term Management
If you need long-term inflammation control, steroids aren’t the only option. For chronic conditions like allergic conjunctivitis or mild uveitis, doctors often turn to:
- NSAID eye drops, like ketorolac or diclofenac-effective for mild inflammation without raising pressure
- Immunosuppressant drops, like cyclosporine (Restasis) or tacrolimus-used for autoimmune eye diseases
- Allergy eye drops, like olopatadine or ketotifen-good for seasonal allergies without steroid risks
For severe autoimmune conditions like sarcoidosis or Vogt-Koyanagi-Harada syndrome, oral steroids or injections might be needed. But even then, eye specialists work closely with rheumatologists to minimize eye exposure.
Final Thoughts: Use Them Wisely, Not Long
Steroid eye drops are powerful tools. They can save your vision when used correctly. But they’re not harmless. The same drops that clear up your red, painful eye can quietly damage your optic nerve or cloud your lens if you use them too long. The key is short-term use, strict monitoring, and knowing when to stop.
If you’ve been prescribed these drops, ask your doctor: "How long should I use them? When will I need a pressure check? What symptoms should I watch for?" Don’t be afraid to push for answers. Your vision is worth it.
Can steroid eye drops cause permanent vision loss?
Yes, if used improperly or without monitoring. The most common cause is steroid-induced glaucoma, where pressure builds up and damages the optic nerve. This damage is often silent-no pain, no symptoms-until significant vision loss occurs. Cataracts from steroids can also permanently blur vision. The good news: both conditions can be prevented with regular eye pressure checks and timely discontinuation of the drops.
How often should I get my eye pressure checked while using steroid drops?
For most people using steroid drops for more than 10 days, pressure should be checked every 2-4 weeks. If you’re on a high-potency drop like Pred Forte, have diabetes, glaucoma, or a family history of glaucoma, your doctor may want you checked every 1-2 weeks. Baseline pressure should always be measured before starting, and a final check is recommended 4-6 weeks after stopping.
Are there steroid eye drops that are safer than others?
Yes. Loteprednol etabonate (Alrex, Lotemax) is a newer steroid designed to break down quickly in the eye, reducing the risk of pressure spikes. It’s often used for short-term inflammation and has a lower association with glaucoma compared to prednisolone acetate or dexamethasone. However, no steroid is completely risk-free. The duration of use matters more than the brand-any steroid used longer than 2-4 weeks increases risk.
Can I use steroid eye drops if I have dry eyes?
Steroid drops can be used for dry eyes if they’re caused by inflammation, like in Sjögren’s syndrome or chronic blepharitis. But they’re not first-line treatment. Artificial tears and non-steroidal anti-inflammatory drops are safer for long-term dry eye. Steroids are reserved for flare-ups and only used briefly under close supervision. Long-term steroid use in dry eye patients can worsen the condition by increasing infection risk and causing corneal thinning.
What happens if I stop steroid eye drops suddenly?
Stopping suddenly can cause rebound inflammation, where your eye condition comes back worse than before. This is especially true for conditions like uveitis or severe allergic conjunctivitis. Your doctor will always taper the dose-reducing frequency gradually over days or weeks-to let your eye adjust. Never stop these drops on your own, even if your symptoms improve.
Do steroid eye drops affect blood sugar or cause weight gain?
Topical steroid eye drops are unlikely to cause systemic effects like weight gain or high blood sugar because so little enters the bloodstream. But with long-term use (over 3-4 weeks), especially with high doses, some absorption can occur. Diabetics should monitor their blood sugar more closely during treatment. While rare, cases of elevated glucose or mood changes have been reported with prolonged use.
Can steroid eye drops cause infections?
Yes. Steroids suppress your eye’s natural immune defenses. This makes you more vulnerable to serious infections like herpes simplex keratitis, fungal keratitis, or bacterial ulcers. These infections can destroy the cornea and lead to blindness if not treated quickly. Never use steroid drops if you have an active infection-your doctor will rule that out first. If your eye gets worse while on steroids, get it checked immediately.
What to Do Next
If you’re currently using steroid eye drops:
- Write down your dosage and start date.
- Call your eye doctor to schedule your next pressure check-even if you feel fine.
- Ask if you’re on a high-risk list for glaucoma or cataracts.
- Don’t share your drops with anyone else. Even a tiny drop can carry infection.
If you’ve used steroid drops in the past and haven’t had an eye exam since:
- Book a comprehensive eye exam. Ask for an intraocular pressure test and optic nerve evaluation.
- Bring your old prescription or bottle to show your doctor.
- Let them know if you’ve had any vision changes since then.
Your eyes don’t warn you before damage happens. But with the right checks, you can use these powerful drops safely-and protect your vision for years to come.

patrick sui
December 3, 2025 AT 00:59Just finished a 6-week course of Pred Forte after uveitis flare-up. Got my IOP checked every 10 days like clockwork - turned out I’m a steroid responder. Pressure hit 32 mmHg. Scary stuff. No symptoms until the optometrist caught it. Glad I didn’t skip appointments. 🙏
Conor Forde
December 3, 2025 AT 13:22So let me get this straight - you’re telling me the same drops that saved my vision are quietly murdering my optic nerve like a silent assassin? 🤯 I’m not mad, I’m just… disappointed. Like my eye’s been dating a narcissist who says ‘I love you’ while stealing my sight. #SteroidDrama
Declan O Reilly
December 4, 2025 AT 04:37It’s wild how medicine walks this razor’s edge - healing one moment, harming the next. We want quick fixes, but the body doesn’t operate on speed. Steroids are like fire: brilliant for warmth, catastrophic if left unattended. The real question isn’t whether they work - it’s whether we’re willing to be patient enough to use them wisely. 🌿
Jeremy Butler
December 6, 2025 AT 04:13It is incumbent upon the patient to engage in rigorous, evidence-based self-monitoring when utilizing corticosteroid ophthalmic formulations. The absence of symptomatic presentation does not equate to the absence of pathophysiological progression. Adherence to scheduled tonometric assessments is not optional; it is a non-negotiable component of therapeutic stewardship.
Adrian Barnes
December 7, 2025 AT 04:55People who don’t get their eye pressure checked every two weeks while on steroids are just gambling with their vision. You think you’re fine? You’re not. You’re just blind to the damage. This isn’t ‘maybe’ - it’s statistical inevitability. If you skipped your follow-ups, you’re lucky you can still see your phone. Stop being lazy and start being responsible.
Declan Flynn Fitness
December 8, 2025 AT 04:35Been using Lotemax for chronic blepharitis - 3 weeks max, then a break. My doc told me: ‘If it feels better, that’s great. But your pressure doesn’t care how you feel.’ So I get checked even when my eyes are chill. You don’t need to suffer to be safe. Stay smart, stay checked. 💪👁️
Patrick Smyth
December 9, 2025 AT 19:59My cousin used steroid drops for 4 months because she ‘felt better.’ Now she’s got cataracts at 34. She didn’t know. No pain. No warning. Just… blurry. Now she needs surgery. Don’t be her. Get checked. NOW.
Linda Migdal
December 11, 2025 AT 15:29Why are we letting foreign pharmaceutical companies dictate how we treat our eyes? In America, we have the best ophthalmologists in the world - yet we still let these dangerous drops go unmonitored? This is negligence. We need mandatory national tracking for steroid eye drop use. No exceptions.
Tommy Walton
December 12, 2025 AT 06:07Reality check: if you’re still using steroid drops after 14 days, you’re not healing - you’re just delaying the inevitable. 🌌 Your eye isn’t a battery. You can’t just ‘charge’ it with chemicals and forget about it. Taper. Switch. Survive.