When you take two drugs at once, you might expect them to work together smoothly. But sometimes, they don’t. One drug can make the other too strong-or even cancel it out entirely. This isn’t a glitch. It’s pharmacodynamic drug interaction, and it’s happening more often than you think. Unlike interactions that change how your body absorbs or breaks down drugs, pharmacodynamic interactions happen right at the target site: the receptor, the cell, or the organ. The drug levels in your blood might be perfect, but the way the drugs talk to each other can still go wrong.
How Drugs Talk to Each Other
Think of drug receptors like locks. Each drug is a key. Some keys fit perfectly and turn the lock to open the door (activate the effect). Others jam the lock (block the effect). And sometimes, two keys work together to open the door faster than either could alone. That’s the heart of pharmacodynamic interactions. There are three main ways drugs interact this way:- Additive: The effect of both drugs together equals the sum of their individual effects. Like taking two painkillers that each give you 50% relief-you end up with 100%.
- Synergistic: The combined effect is stronger than the sum. It’s not 50% + 50% = 100%. It’s 50% + 50% = 180%. This is why some antibiotic combos work so well.
- Antagonistic: One drug blocks or reduces the effect of the other. This isn’t just about being less effective-it can be dangerous.
Receptor Competition: When Drugs Fight for the Same Spot
One of the most common and dangerous types happens when two drugs compete for the same receptor. Take asthma meds. Albuterol, a beta-2 agonist, opens up airways by binding to beta-2 receptors in the lungs. But if you’re also taking propranolol, a beta-blocker used for high blood pressure or heart rhythm problems, it binds to those same receptors-tightly. Propranolol doesn’t just slow your heart rate; it can completely block albuterol from working. The result? A patient with asthma might not respond to their rescue inhaler during an attack. This isn’t theoretical. It’s happened in emergency rooms across Australia and the US. The key here isn’t dose-it’s affinity. The drug with higher receptor affinity wins. Propranolol has a higher affinity for beta receptors than albuterol. Even small doses can shut down the effect. This is why doctors avoid prescribing beta-blockers to people with asthma, unless they’re using cardioselective ones (like metoprolol) that mostly target the heart.Physiological Antagonism: Indirect but Deadly
Not all interactions happen at the same receptor. Sometimes, drugs affect different systems that end up working against each other. A classic example: NSAIDs like ibuprofen and ACE inhibitors like lisinopril. ACE inhibitors help lower blood pressure by relaxing blood vessels and reducing fluid retention. But NSAIDs block prostaglandins-chemicals that help keep blood flowing to the kidneys. When you take both, the NSAID cuts kidney blood flow by about 25%, according to a 2019 NIH study. The ACE inhibitor loses its ability to protect kidney function. Blood pressure doesn’t drop. Kidneys get stressed. In older adults, this combo can lead to sudden kidney failure. It’s not rare. The NHS Specialist Pharmacy Service lists this as one of the top 10 potentially harmful interactions. Another example: diuretics (water pills) and NSAIDs. The diuretic flushes out fluid. The NSAID tells the kidneys to hold onto it. The result? Swelling, high blood pressure, and no relief from either drug.The Dangerous Duo: Serotonin Syndrome and Opioid Overdose
Some pharmacodynamic interactions are life-threatening. One of the most feared is serotonin syndrome. It happens when two drugs that boost serotonin are taken together-like an SSRI (e.g., sertraline) with an MAOI (e.g., phenelzine). The brain gets flooded with serotonin. Symptoms: confusion, rapid heartbeat, high fever, muscle rigidity. A 2021 meta-analysis found this combo increases serotonin syndrome risk by 24 times. It’s why doctors wait at least two weeks after stopping an MAOI before starting an SSRI. Another deadly combo: opioids and opioid antagonists. Naloxone (Narcan) is used to reverse opioid overdoses. But if someone is physically dependent on opioids and gets naloxone accidentally-say, during surgery-it can trigger full withdrawal: vomiting, seizures, high blood pressure. It’s not just unpleasant. It can be fatal.
When Drugs Work Better Together
Not all pharmacodynamic interactions are bad. Sometimes, they’re intentional. Trimethoprim and sulfamethoxazole (Bactrim) are a perfect example. Each blocks a different step in the bacteria’s folic acid production. Together, they’re far more effective than either alone-cutting the needed dose by 75%. This synergy is why it’s still a first-line treatment for urinary tract infections. Another emerging use is low-dose naltrexone (LDN) with antidepressants. A 2021 study in the Journal of the American Pharmacists Association showed that adding LDN to standard antidepressants improved treatment-resistant depression in 68% of patients-compared to 42% with antidepressants alone. The theory? Naltrexone briefly blocks opioid receptors, triggering the body to produce more natural endorphins. It’s not mainstream yet, but it’s a sign that we’re learning to use these interactions wisely.Why Some People Are at Higher Risk
You don’t need to be on ten drugs to be at risk. The biggest danger comes from drugs with a narrow therapeutic index-meaning the difference between a helpful dose and a toxic one is tiny. Think warfarin (blood thinner), digoxin (heart drug), or lithium (mood stabilizer). A small change in how these drugs act can mean the difference between safety and hospitalization. A 2019 NIH analysis found that 83% of life-threatening pharmacodynamic interactions involved at least one drug with a therapeutic index below 3.0. Older adults are especially vulnerable. The average person over 65 takes 4.8 prescription drugs, according to 2022 data. Combine that with slower metabolism, reduced kidney function, and multiple chronic conditions, and the chances of a bad interaction skyrocket.What Doctors and Pharmacists Are Doing About It
Clinical decision support tools in hospitals now flag potential interactions. But they’re not perfect. A 2020 study in Drug Safety found they still miss 22% of serious pharmacodynamic interactions because they’re programmed to look for simple rules, not complex physiology. The most effective solution? Pharmacist-led reviews. A 2021 review in BMJ Quality & Safety showed that when pharmacists actively review medication lists-especially in elderly patients-they prevent 58% of adverse events from drug interactions. The most common ones they catch? NSAIDs with blood pressure meds, and multiple sedatives (like benzodiazepines, opioids, and sleep aids) taken together. In Australia, hospitals are starting to integrate interaction alerts directly into electronic prescribing systems. But knowledge still matters more than software. A 2022 survey of 1,247 doctors found 63% encountered a dangerous interaction at least once a month. The top culprits? Anticoagulants with antiplatelets (like aspirin and warfarin), and CNS depressants (alcohol, opioids, benzodiazepines).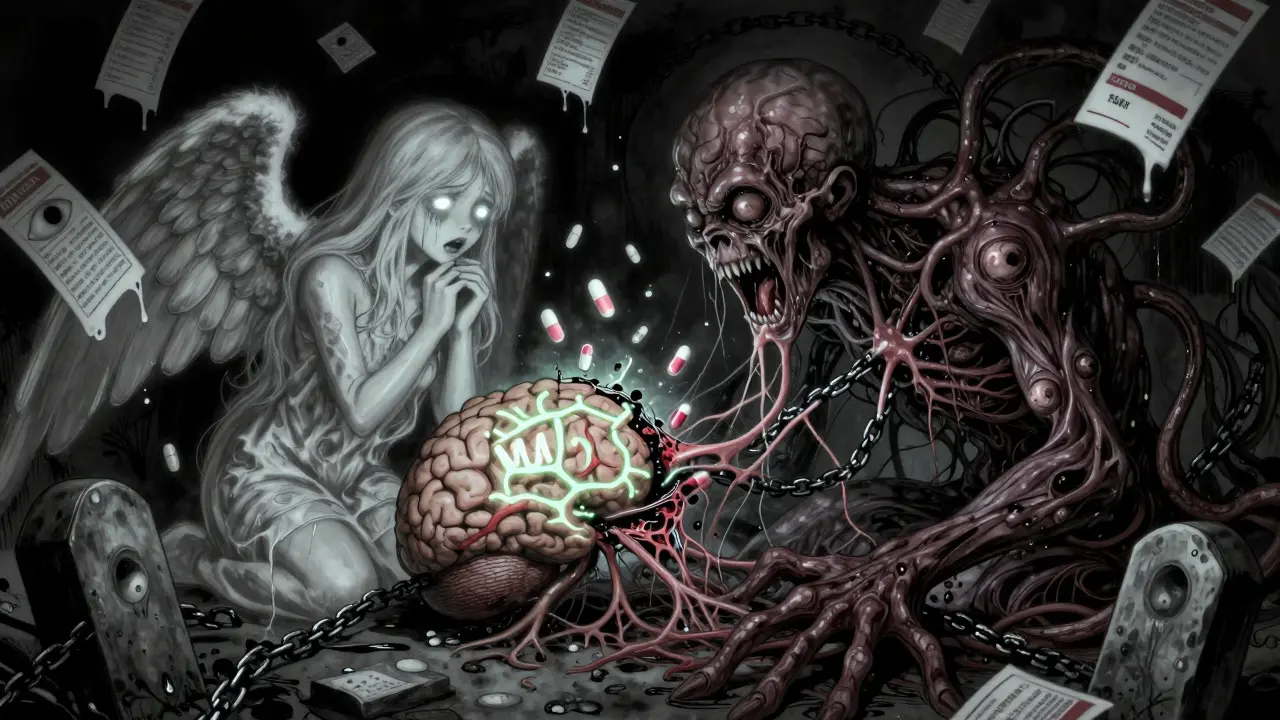
What You Can Do
You don’t need to be a doctor to protect yourself. Here’s how:- Keep a list: Write down every medication you take-including supplements, OTC painkillers, and herbal products. Bring it to every appointment.
- Ask: When a new drug is prescribed, ask: “Could this interact with anything I’m already taking?”
- Don’t assume: Just because something is “natural” doesn’t mean it’s safe. St. John’s Wort can reduce the effect of birth control pills, antidepressants, and even some heart meds.
- Use one pharmacy: It helps pharmacists track everything you’re on and spot risks.
What’s Coming Next
The future of drug safety is moving beyond checklists. Researchers are building machine learning models that predict interactions based on how drugs affect biological pathways-not just receptor names. Dr. Rada Savic’s team at UCSF developed an algorithm that predicts serotonin syndrome risk with 89% accuracy. The UK’s NHS is piloting real-time alerts in electronic health records that don’t just say “warning,” but explain why: “Ibuprofen reduces kidney blood flow, which may block lisinopril’s effect.” The European Medicines Agency now requires pharmacodynamic interaction studies for 34% of new drug applications-up from 19% in 2015. The FDA has started requiring this for all new CNS drugs. Why? Because we’re getting smarter. And we’re running out of time. By 2050, 1.5 billion people will be over 65. Most will be on multiple drugs. Understanding how they interact won’t be optional-it’ll be essential.What’s the difference between pharmacodynamic and pharmacokinetic drug interactions?
Pharmacokinetic interactions change how your body processes a drug-like how fast it’s absorbed, broken down, or cleared. For example, grapefruit juice slows down the enzyme that breaks down statins, raising their blood levels. Pharmacodynamic interactions happen at the target site: the drug’s effect is changed even if its concentration stays the same. One drug might block a receptor, boost a chemical, or interfere with a body system. The drug level is fine-but the result is wrong.
Can over-the-counter drugs cause pharmacodynamic interactions?
Absolutely. Common OTC drugs like ibuprofen, naproxen, and even antihistamines can cause serious interactions. Ibuprofen can reduce the effectiveness of blood pressure meds. Diphenhydramine (Benadryl) adds to the sedative effect of opioids or sleep aids, increasing fall risk. Even herbal supplements like St. John’s Wort can block the effect of antidepressants or birth control. Never assume OTC means safe.
Are pharmacodynamic interactions more dangerous than pharmacokinetic ones?
They can be. While pharmacokinetic interactions are more common (about 60% of cases), pharmacodynamic ones are more likely to cause serious harm. A 2020 analysis found that 68% of hospitalizations from drug interactions were due to pharmacodynamic causes, compared to 42% from pharmacokinetic ones. Why? Because you can’t always fix them by lowering the dose. Sometimes, the only safe option is to stop one drug entirely.
Why do some drug combinations work better together?
Sometimes, drugs target different steps in the same process. For example, trimethoprim and sulfamethoxazole block two different enzymes in bacterial folic acid production. Together, they shut it down completely. This synergy means lower doses of each drug are needed, reducing side effects. These combinations are carefully designed and tested-unlike accidental interactions, which are unpredictable and often harmful.
Can pharmacodynamic interactions be predicted?
Yes, but not perfectly. Standard drug interaction databases list known risks, but they miss complex, indirect effects. Newer tools use machine learning to model how drugs affect biological pathways-not just receptors. A 2022 study showed these models predict serotonin syndrome risk with 89% accuracy. Still, human judgment is key. Pharmacists who review medication lists catch risks that software misses.

