Combining opioids with MAOIs isn’t just risky-it’s potentially fatal. This isn’t a hypothetical warning. It’s a documented pattern of death, hospitalizations, and near-misses that have been known for over 60 years. Yet, every year, patients on these antidepressants still get prescribed dangerous painkillers. Why? Because many providers don’t know the full danger, and patients often don’t realize their antidepressant could turn a routine pain pill into a life-threatening event.
What Happens When Opioids and MAOIs Mix?
Monoamine oxidase inhibitors (MAOIs) like phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan) work by blocking enzymes that break down key brain chemicals: serotonin, norepinephrine, and dopamine. That’s how they help with depression. But when you add certain opioids, you’re essentially flooding the system with more of those same chemicals. The result? A runaway cascade. The two biggest dangers are serotonin syndrome and hypertensive crisis. Serotonin syndrome happens when your brain gets too much serotonin. Symptoms start fast-sometimes within an hour: high fever (over 104°F), muscle rigidity, confusion, seizures, rapid heartbeat, and sweating. In severe cases, it leads to organ failure and death. Hypertensive crisis is a sudden, dangerous spike in blood pressure, often above 200/120 mmHg, which can cause stroke or heart attack. A 2017 study in the British Journal of Clinical Pharmacology showed that meperidine (Demerol) combined with an MAOI can boost serotonin levels by 300-500% in under an hour. That’s not a minor uptick. That’s a toxic surge.Which Opioids Are Most Dangerous?
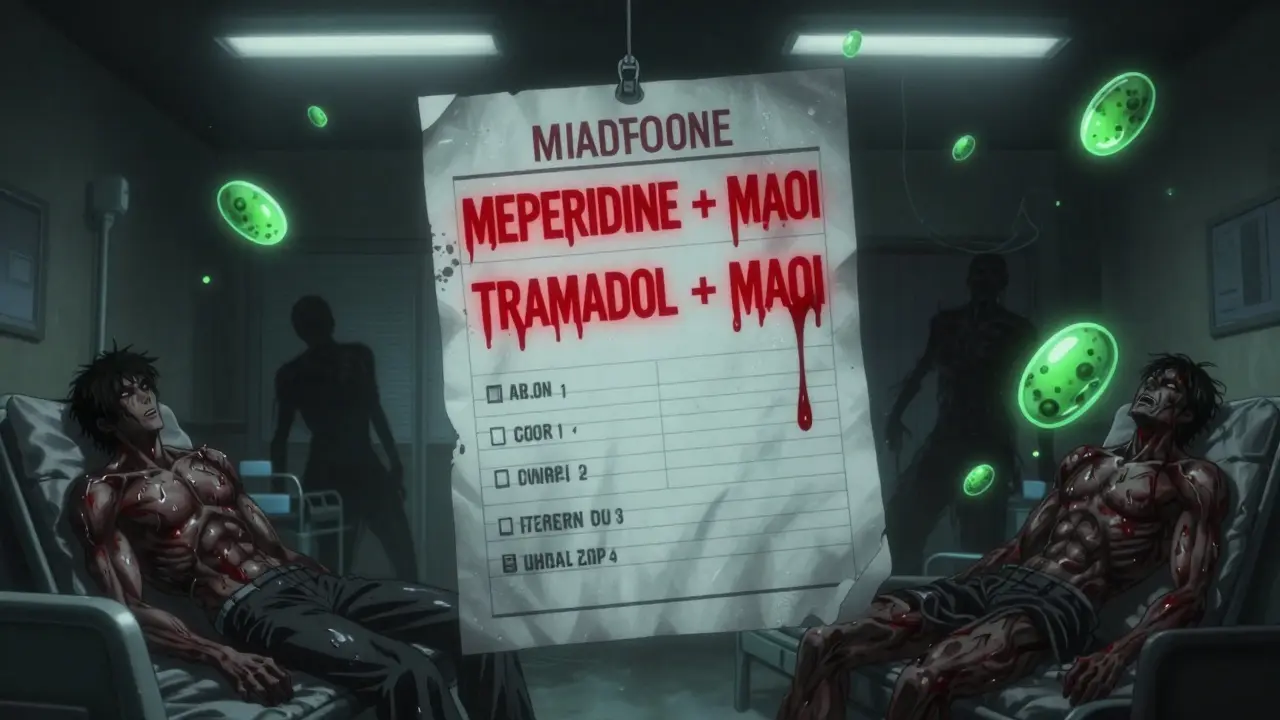
Not all opioids are created equal when it comes to MAOIs. Some are outright banned. Others are risky. A few are safer-but still require caution.- Meperidine (Demerol): The worst offender. Between 1960 and 2010, there were 37 documented deaths from this combo. The FDA has a black box warning. It’s absolutely contraindicated.
- Tramadol: Often mistaken as “safe” because it’s not a traditional opioid. But it blocks serotonin reuptake. There are 21 confirmed cases of serotonin syndrome with MAOIs. A Reddit user on r/antidepressants described a 107.1°F fever, muscle rigidity, and seizures after taking tramadol for dental pain while on phenelzine. They spent 72 hours in ICU.
- Methadone: Has serotonin effects and NMDA antagonism. Moderate risk. Case reports exist. Avoid unless no other option.
- Tapentadol (Nucynta): Similar to tramadol. Purdue Pharma paid a $4.7 million settlement in 2021 for failing to warn about this interaction.
- Morphine, hydromorphone, oxycodone: Lower risk, but not zero. They don’t directly affect serotonin, but can still contribute to CNS depression or indirect serotonin release. Use only if essential and under close supervision.
- Buprenorphine: The safest opioid option for MAOI users. Studies show no serotonin syndrome cases in over 140 administrations at low doses (0.2-0.4 mg sublingual). It’s the go-to for acute pain in these patients.
How Long Do You Have to Wait After Stopping an MAOI?
This is critical. You can’t just stop your MAOI and start an opioid the next day. MAOIs permanently disable the enzymes they bind to. Your body needs time to grow new ones. For irreversible MAOIs like Nardil or Parnate, you need a 14-day washout period before starting any opioid with serotonergic activity. This isn’t a suggestion-it’s a medical requirement. The FDA’s 2022 labeling for selegiline (Emsam) patch confirms this. Even if you feel fine, your enzymes aren’t back online yet. Reversible MAOIs like moclobemide (Aurorix) are different. They detach from the enzyme after a few hours. For these, a 24-hour gap is usually enough. But even then, caution is advised. There are still case reports of serotonin syndrome with moclobemide and tramadol.
What Should You Use Instead of Opioids?
If you’re on an MAOI and need pain relief, you have options-just not the ones most people assume.- Buprenorphine: As mentioned, it’s the safest opioid choice. Use low doses and monitor closely.
- Acetaminophen (Tylenol): No interaction with MAOIs. Safe for mild to moderate pain.
- NSAIDs: Ibuprofen, naproxen, celecoxib-all safe. Avoid if you have kidney or stomach issues.
- Non-drug options: Physical therapy, ice/heat, acupuncture, nerve blocks. These are underused but effective.
Never use tramadol, meperidine, methadone, or tapentadol. Even if your doctor says “it’s just a small dose,” the risk isn’t dose-dependent. It’s mechanism-dependent. One pill can be enough.
Why Do These Mistakes Keep Happening?
You’d think this would be a closed case by now. But here’s the reality:- Tramadol is still prescribed as a “non-narcotic” painkiller. Many patients don’t realize it’s an opioid.
- Primary care doctors prescribe 63% of these dangerous combinations, according to a 2021 study in the Journal of Clinical Psychiatry.
- Emergency rooms see 18.7% of MAOI patients presenting with opioid-related complications.
- A 2022 study in JAMA Internal Medicine found that 4.3% of MAOI users got a contraindicated opioid within 14 days of starting the drug. That’s about 11,200 dangerous prescriptions every year in the U.S. alone.
- Even with electronic health record alerts, 14.3% of warnings are overridden. That means someone clicked past the red flag.
And here’s the scariest part: 31% of emergency physicians surveyed in 2022 didn’t know tramadol was contraindicated with MAOIs. That’s not a patient error. That’s a system failure.
What Should You Do as a Patient?
If you’re on an MAOI, here’s your action plan:- Know your meds. If you’re on Nardil, Parnate, or Marplan, you’re at risk. Don’t assume your pain doctor knows.
- Carry a wallet card. The National Alliance on Mental Illness (NAMI) offers free cards listing contraindicated drugs. 78% of patients who carry them say it’s helped them avoid errors.
- Always tell every provider you see-dentists, ER staff, physical therapists-that you’re on an MAOI. Don’t assume they’ll check your chart.
- Ask: “Is this an opioid? Does it affect serotonin?” If they say “it’s not a real opioid,” push back. Tramadol and tapentadol are opioids.
- Wait 14 days after stopping your MAOI before taking any opioid. Even if you feel better, your body isn’t ready.

What Should Providers Do?
For doctors, pharmacists, and nurses:- Use hard-stop alerts in your EHR. Epic Systems blocked over 8,000 dangerous prescriptions in 2021. Don’t override them without a clear, documented reason.
- When a patient on an MAOI needs pain relief, default to buprenorphine, acetaminophen, or NSAIDs.
- Know the 12 opioids the FDA specifically warns against in MAOI patients: meperidine, tramadol, methadone, tapentadol, dextromethorphan, fentanyl (in high doses), oxymorphone, codeine (in some cases), hydrocodone (in some cases), and more.
- Don’t rely on patient memory. Confirm with their pharmacy records.
There’s a digital tool now called SerotoninSafe, approved by the FDA in 2023. It integrates with EHRs and gives real-time alerts. In a pilot at Johns Hopkins, it cut prescribing errors by 76%. If your hospital doesn’t have it, ask why.
What to Do in an Emergency
If someone on an MAOI develops fever, rigidity, confusion, or rapid heart rate after taking an opioid:- Call 911 immediately.
- Do NOT give more painkillers.
- Ask if they’ve taken any new meds in the last 24 hours.
- At the hospital, treatment includes cyproheptadine (12mg loading dose), benzodiazepines for seizures or agitation, and active cooling.
- They need ICU-level monitoring for at least 24 hours.
Time is everything. Serotonin syndrome can go from mild to fatal in under 12 hours.
The Bigger Picture
MAOIs are no longer first-line antidepressants. They make up less than 1% of prescriptions. But they’re still vital for treatment-resistant depression-about 1.2 million people in the U.S. still use them. That means 1.2 million people are walking around with a ticking time bomb in their medicine cabinet. Pharmaceutical companies have been sued. Regulators have issued warnings. Hospitals have built digital barriers. Yet, mistakes still happen. Why? Because the system assumes patients will know, doctors will remember, and pharmacists will catch it. But humans forget. Systems glitch. Labels get ignored. The truth is simple: MAOIs and most opioids don’t mix. Period. There’s no safe gray area. No “just this once.” No “low dose.” If you’re on one, you need to know the list of drugs you must avoid-and you need to make sure every provider you see knows it too.The science is clear. The warnings are loud. The deaths are documented. Now it’s up to you to make sure you or someone you care about isn’t the next statistic.
Can I take tramadol if I’m on an MAOI?
No. Tramadol is one of the most dangerous opioids to combine with MAOIs. It blocks serotonin reuptake, and MAOIs prevent serotonin breakdown. Together, they can cause serotonin syndrome-a medical emergency with symptoms like high fever, muscle rigidity, seizures, and death. Over 68 cases have been reported to the WHO since 2010, and many ended in ICU stays or fatalities. Never take tramadol while on an MAOI, even for short-term pain.
How long after stopping an MAOI can I safely take an opioid?
For irreversible MAOIs like phenelzine or tranylcypromine, you must wait 14 days after your last dose before starting any opioid with serotonergic activity. This is because MAO enzymes take about two weeks to regenerate. For reversible MAOIs like moclobemide, a 24-hour gap is usually sufficient, but only under medical supervision. Never assume you’re safe after just a few days.
Is buprenorphine safe with MAOIs?
Yes, buprenorphine is the safest opioid option for people on MAOIs. Studies have shown no cases of serotonin syndrome in over 140 administrations when used at low doses (0.2-0.4 mg sublingual). It’s now recommended by the American Society of Anesthesiologists for acute pain in MAOI patients. Still, monitor for respiratory depression, especially if you’re also on benzodiazepines.
What painkillers are safe with MAOIs?
Safe options include acetaminophen (Tylenol), ibuprofen, naproxen, and other NSAIDs (if no kidney or stomach issues). Buprenorphine is the only opioid considered safe at low doses. Avoid all other opioids-including codeine, hydrocodone, oxycodone, methadone, tramadol, tapentadol, and meperidine. Even “mild” opioids carry risk. Stick to non-opioid options unless absolutely necessary and under expert supervision.
Can I use dextromethorphan (in cough syrup) with an MAOI?
No. Dextromethorphan is a cough suppressant that also affects serotonin. The FDA explicitly lists it as contraindicated with MAOIs. Even small amounts in over-the-counter cough syrups can trigger serotonin syndrome. Always check labels and ask your pharmacist. Many cold and flu products contain dextromethorphan-never assume they’re safe.
What should I do if I accidentally took an opioid while on an MAOI?
Seek emergency medical help immediately. Do not wait for symptoms. Serotonin syndrome can develop within 1-2 hours. If you experience fever, muscle stiffness, confusion, rapid heartbeat, or seizures, call 911. Tell responders you’re on an MAOI and took an opioid. Time is critical. Emergency treatment includes cyproheptadine, benzodiazepines, cooling, and ICU monitoring.
Are there any new treatments or tools to prevent this interaction?
Yes. The FDA approved a digital tool called SerotoninSafe in 2023 that integrates with electronic health records to flag dangerous drug combinations in real time. In a pilot at Johns Hopkins, it reduced prescribing errors by 76%. Hospitals are also implementing hard stops in their prescribing systems. Still, community pharmacies and primary care settings lag behind. Patient education tools like NAMI’s wallet cards remain vital.

Henriette Barrows
December 30, 2025 AT 05:30This is the kind of post that saves lives. I’ve seen too many people assume ‘it’s just a little tramadol’-like it’s harmless. It’s not. My cousin ended up in the ICU after a dentist prescribed it for a root canal. She was on phenelzine and didn’t even know it was an opioid. Please, if you’re on an MAOI, treat this like a bomb squad manual. Share this. Save someone.
David Chase
December 31, 2025 AT 04:55THIS IS WHY AMERICA IS DYING. 🚨
Doctors are lazy. Patients are dumb. Pharmacies don’t check. And now we got people popping tramadol like it’s Advil while on Nardil like it’s a fucking TikTok trend. I’ve seen three obituaries for this exact combo in the last year. The FDA’s been screaming for decades. Why is this still happening? Because no one gives a shit until it’s their kid in the ICU. #WakeUpAmerica
Kevin Lopez
December 31, 2025 AT 08:07MAOI-opioid pharmacodynamics are non-linear and serotonergically synergistic. The 14-day washout is non-negotiable due to irreversible MAO-A inhibition and enzyme turnover kinetics. Tramadol’s SNRI activity + MAOI = 5-HT syndrome risk multiplier. Buprenorphine’s partial agonism and low efficacy profile render it the only viable opioid alternative. Case closed.
Teresa Rodriguez leon
January 1, 2026 AT 10:45My ex was on Parnate. He took tramadol for a back flare-up. He died in his sleep. No warning. No signs. Just… gone. I’ve been screaming into the void for years. No one listens. No one cares. Until it’s your loved one. Then it’s too late.
Sharleen Luciano
January 2, 2026 AT 04:33How is it still 2024 and we’re having this conversation? The literature on this interaction has been peer-reviewed since the 1960s. The FDA issued black box warnings in the 90s. We have AI-driven EHR systems now. Yet, primary care physicians still prescribe tramadol like it’s a vitamin. This isn’t negligence-it’s institutional arrogance. And patients? They’re too trusting. They assume their doctor knows. They don’t realize that most doctors are just following algorithmic prompts that override their own training. We’ve outsourced critical thinking to tech that’s still stuck in 2010.
It’s not just about the drugs. It’s about the erosion of clinical judgment. The medical industrial complex wants quick fixes. Quick scripts. Quick profits. Not patient safety. Not long-term outcomes. Just volume. And so we get 11,200 dangerous prescriptions a year-not because of ignorance, but because the system incentivizes compliance over caution.
And don’t get me started on dextromethorphan. People think it’s ‘just a cough syrup.’ It’s a serotonergic agent with a half-life longer than your attention span. It’s in Robitussin. It’s in NyQuil. It’s in every damn cold medicine at CVS. And no one checks the label. Why? Because we’ve been conditioned to believe that OTC means ‘safe.’ It doesn’t. It means ‘profitable.’
Meanwhile, buprenorphine is the gold standard. Underused. Undervalued. Overshadowed by the opioid crisis narrative that paints all opioids as villains. But here’s the truth: not all opioids are equal. And treating them as such is the real danger. We need better education. Better labeling. Better systems. Not just more warnings that get clicked away.
And yes, I’m the person who prints out the NAMI card and carries it in my wallet. I’ve shown it to ER nurses. I’ve handed it to dentists. I’ve had people roll their eyes. But I’ve also saved lives. Because if you’re not advocating for yourself, no one else will.
This isn’t fearmongering. It’s pharmacology. And if you’re not treating it with the gravity it deserves, you’re not just irresponsible-you’re complicit.
Fabian Riewe
January 2, 2026 AT 06:06Big thank you to the OP for laying this out so clearly. I’m a nurse and I’ve seen this go sideways too many times. Last month, a guy came in with fever and rigidity after taking tramadol for a toothache. He was on moclobemide. He didn’t even know it was an MAOI-he thought it was ‘just another antidepressant.’ We had to intubate him. He’s fine now, but it was terrifying.
One thing I tell patients: if your doctor says ‘it’s not a real opioid,’ ask them to define ‘real.’ Tramadol is an opioid. Tapentadol is an opioid. Dextromethorphan? Also an opioid in disguise. They’re not just ‘painkillers’-they’re serotonin grenades. And MAOIs are the fuse.
Also, if you’re on an MAOI, tell every provider. Even the acupuncturist. Even the chiropractor. Even the guy at the pharmacy who hands you your prescription. Don’t assume they’ll check. They won’t.
Amy Cannon
January 2, 2026 AT 16:58As someone who grew up in India and moved to the US five years ago, I was stunned by how casually some doctors here treat medication interactions. Back home, if you were on an MAOI, your entire family would know not to touch any painkiller without checking with the pharmacist. Here? People just grab whatever’s on the shelf. I had to correct my neighbor’s doctor when he prescribed tramadol to her for migraines-she was on phenelzine. He said, ‘Oh, it’s fine, she’s only taking one pill.’ I almost cried. That’s not how this works. I’ve been sharing this post with every Indian expat group I’m in. We need to protect each other.
Alex Ronald
January 3, 2026 AT 23:49Just want to add a practical tip: if you’re on an MAOI, keep a printed list of contraindicated drugs in your wallet, phone, and on your fridge. I made mine with big bold letters: TRAMADOL, MEPERIDINE, TAPENTADOL, DEXTROMETHORPHAN - NO. BUPRENORPHINE - OK. ACETAMINOPHEN - OK. NSAIDS - OK. I showed it to my pharmacist last week. He said, ‘I wish more patients did this.’ You’d be surprised how many pharmacists don’t catch it either. Be your own advocate. It’s not paranoia. It’s survival.
Himanshu Singh
January 4, 2026 AT 14:45thanks for this post! i was on moclobemide and took a cough syrup with dextromethorphan last year. i got dizzy and nauseous but thought it was just the flu. now i know it was serotonin syndrome. i’ve been scared to take anything since. i’m going to print this out and show my doctor. thank you thank you thank you.
Jasmine Yule
January 4, 2026 AT 19:05I’ve been on Nardil for 8 years. I had a back injury last year and was terrified to ask for pain relief. I spent weeks researching. I printed this exact post and gave it to my pain specialist. He said, ‘You’re the first patient who came in with this.’ I cried. Not because I was scared-but because I felt seen. If you’re reading this and you’re on an MAOI: you’re not alone. You’re not overreacting. You’re not being dramatic. You’re being smart. Keep fighting. Keep speaking up. And if you’re a provider? Read this. Then listen.
Greg Quinn
January 5, 2026 AT 00:55There’s a deeper irony here: we live in a world that worships individual responsibility-‘take ownership of your health!’-but the system is designed to make that impossible. You’re supposed to know that tramadol is an opioid, that MAOIs don’t clear in 48 hours, that dextromethorphan is a chemical trap. But no one teaches you this in school. No one explains it in plain language in the pharmacy. The burden falls on the patient, while the system remains oblivious. This isn’t just about drugs. It’s about power. Who gets to decide what’s safe? And why is that decision so often made without the person who has to live with the consequences?
Nicole K.
January 6, 2026 AT 03:39So you’re saying it’s okay to use buprenorphine? That’s just another drug addict’s medicine. Why not just tough it out? You’re on an antidepressant anyway-you should be strong enough to handle pain without drugs. This is why people are so weak these days. Just say no to opioids. Always.