Medication Substitution Assistant
Find Safe Drug Alternatives
When your medication is unavailable, this tool helps identify appropriate alternatives with dosing guidance and safety considerations based on real-world shortage data.
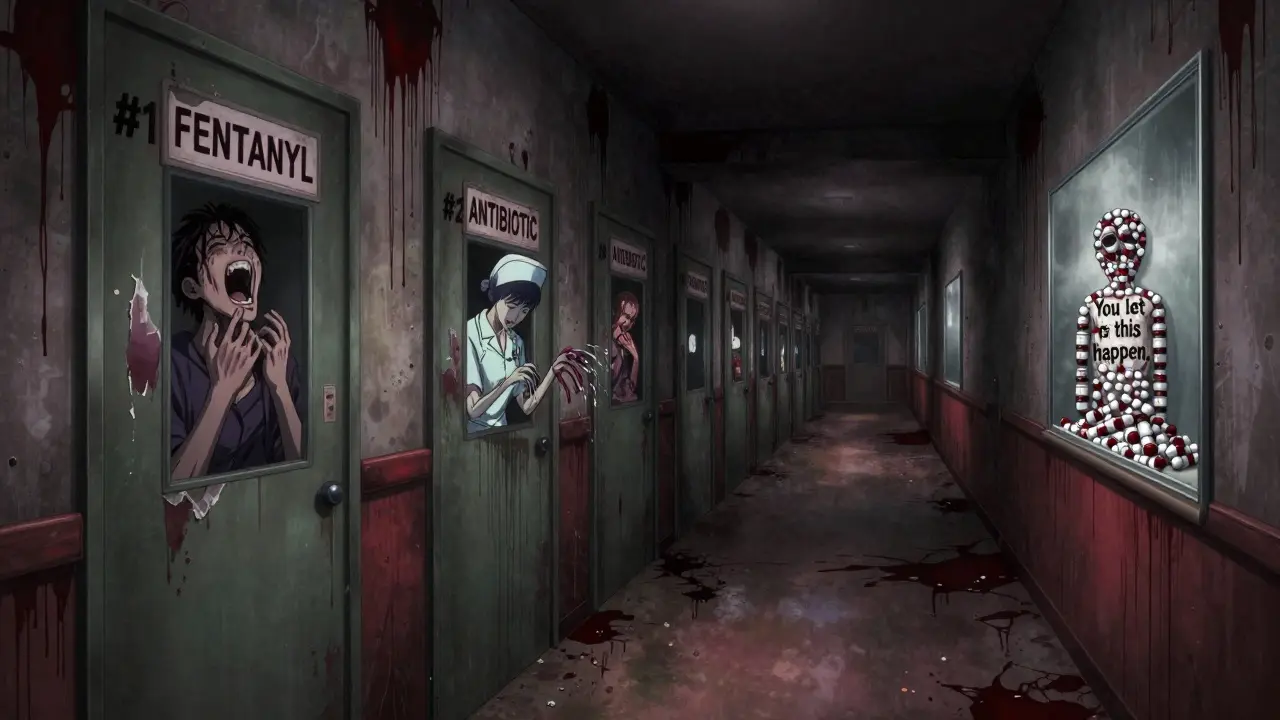
When a life-saving drug suddenly disappears from the shelf, it’s not just an inconvenience-it’s a crisis. Hospitals scramble. Patients delay treatment. Nurses work extra hours. And sometimes, lives are put at risk. Medication shortages aren’t rare glitches-they’re a growing, systemic problem in U.S. healthcare. In 2022 alone, there were 287 documented drug shortages, affecting nearly one in five essential medications used in hospitals. This isn’t about running out of cough syrup. This is about not having morphine for post-surgery pain, saline for IVs, antibiotics for infections, or chemotherapy drugs for cancer patients. And the problem is getting worse.
Why Medication Shortages Happen
Most people assume drug shortages happen because of supply chain delays or natural disasters. But the real cause is more structural-and it’s rooted in how generic drugs are made and paid for. Over 63% of all drug shortages involve generic sterile injectables: things like IV antibiotics, cancer drugs, anesthesia agents, and saline solutions. These aren’t fancy, high-profit medications. They’re cheap, high-volume, and made by just a few manufacturers. In fact, three companies control 75% of the production capacity for these critical drugs.
When one of those factories has a quality issue-a contaminated batch, a broken machine, or a failed inspection-the entire supply chain stalls. Manufacturing quality problems caused 46% of shortages in 2022. That’s not a fluke. It’s a pattern. And because these drugs are sold at rock-bottom prices, manufacturers have little incentive to invest in backup equipment, redundant production lines, or better quality control. The system is built to run on thin margins, and when something breaks, there’s no safety net.
Adding to the problem: 80% of the active ingredients in U.S. drugs come from overseas, mostly China and India. A single regulatory inspection delay in one foreign facility can ripple across dozens of medications. Meanwhile, the U.S. has no national strategic stockpile for everyday medications, unlike countries like Germany or Canada, which keep buffer inventories of critical drugs. When a shortage hits here, hospitals are left to fend for themselves.
How Shortages Impact Patients and Providers
The human cost is real. A 2023 study from the American College of Physicians found that 78% of safety-net hospitals-those serving Medicaid and uninsured patients-had to cancel or delay procedures because of missing drugs. Rural clinics? They’re hit hardest. No nearby pharmacy? No backup supplier? That means no treatment.
For doctors, it’s a nightmare. You know a patient needs a specific drug. You write the prescription. But when you call the pharmacy, they say, “We don’t have it.” Now you’re playing medical chess: What’s the alternative? Is it safe? Is it covered? Will it cause side effects? In one case documented by pharmacists on Reddit, a shortage of morphine forced staff to switch to hydromorphone. The result? A 15% spike in medication errors during the transition.
Nurses are stretched even thinner. According to the American Journal of Nursing, patient wait times for critical medications increased by an average of 22 minutes during shortages. That might not sound like much, but in an ER or ICU, minutes can mean the difference between recovery and collapse. And pharmacy teams? They’re working an extra 12.7 hours per week on average, just to track down substitutes, adjust dosing, and update records.

What Hospitals Are Doing to Cope
Hospitals aren’t sitting idle. The most effective ones have built formal shortage response teams. These aren’t ad-hoc committees. They’re permanent groups with clear roles: a pharmacy lead, a nurse representative, an IT specialist, a risk manager, and a communications officer. Their job? To act before the shortage hits the news.
Here’s how they do it:
- They monitor supply chains daily-not just for drugs they use, but for their alternatives too.
- They track inventory levels in real time, with systems that flag when stock drops below 14 days of supply.
- They pre-approve substitution protocols so nurses don’t have to wait for a doctor’s order when a drug vanishes.
- They conduct quarterly drills: “What if we lose fentanyl for a month?” Simulations cut medication errors by 33% during real shortages.
But not all hospitals can afford this. Only 35% of safety-net hospitals maintain even 14 days of buffer inventory. Most are stuck with 8 to 12 days-barely enough to cover a week of delays. And when the shortage lasts longer? That’s when patients suffer.
Why Alternatives Aren’t Always Safe
When a drug disappears, the go-to solution is substitution. But not all substitutes are created equal. Take vancomycin, a common antibiotic. If it’s unavailable, some hospitals switch to daptomycin. But daptomycin costs 10 times more, requires different dosing, and can’t be used in patients with kidney issues. Another example: when phenylephrine (a blood pressure drug) went into shortage, providers turned to norepinephrine. But norepinephrine must be given through a central line, not a regular IV. That means more procedures, more risks, and more training.
And then there’s the issue of dosing. A 2023 study in the Journal of Hospital Medicine found that when pharmacists switched patients from one brand of insulin to another due to shortage, 21% of patients had blood sugar levels that went out of target range in the first week. Why? Because even “equivalent” drugs aren’t always interchangeable. Their absorption, timing, and side effect profiles vary. And without clear guidance, clinicians are guessing.
What Needs to Change
Band-aid fixes won’t solve this. We need systemic change. Here’s what experts are calling for:
- Reform Medicare reimbursement. Right now, hospitals get paid the same for a $0.50 generic drug as they do for a $500 specialty drug. That disincentivizes manufacturers from making reliable, low-cost products. Experts like former FDA Commissioner Dr. Scott Gottlieb argue that Medicare should reward manufacturers who maintain consistent, high-quality supply chains.
- Create a national strategic stockpile. Germany keeps six months’ supply of critical injectables. The U.S. has nothing beyond the Strategic National Stockpile-which is only for bioterrorism and pandemics, not everyday shortages.
- Require mandatory reporting. In the U.S., manufacturers only report shortages voluntarily. Only 65% comply. Countries like France and Canada require reporting within 48 hours of a disruption. That cuts shortage duration by 37%.
- Invest in advanced manufacturing. New technologies can switch production lines from one drug to another in hours, not weeks. If just half of U.S. manufacturers adopted this, shortage frequency could drop by 40%.
The economic cost is staggering. Hospitals spend an average of $218,000 per year managing each shortage. That’s $1.2 billion industry-wide. And that’s just the direct cost. The hidden cost? Delayed surgeries, worsened outcomes, longer hospital stays, and preventable deaths.
What You Can Do
If you’re a patient, you can’t fix the system. But you can protect yourself:
- Ask your doctor: “Is this drug in shortage? Are there alternatives?”
- If you’re on a chronic medication, keep a 30-day supply on hand if possible.
- Sign up for pharmacy alerts-some chains notify customers when a drug is running low.
- Don’t assume your insurance will cover a substitute. Always check.
If you’re a provider, advocate for your hospital to build a shortage response team. Push for better inventory tracking. Demand training. And don’t wait for a crisis to act. Proactive monitoring reduces stress-and saves lives.
Medication shortages aren’t going away. But they’re not inevitable. They’re the result of choices-about pricing, regulation, manufacturing, and prioritization. Fixing them means rethinking how we value essential medicines. Not as commodities. Not as line items on a budget. But as lifelines.
Why are generic drugs more likely to be in shortage than brand-name drugs?
Generic drugs are more likely to be in shortage because they’re low-margin products made by a small number of manufacturers. Since they sell for pennies, companies don’t invest in backup production lines, quality systems, or inventory buffers. Brand-name drugs, by contrast, are often made by a single company with higher profit margins, so they can afford to maintain redundancy. In 2022, 63% of all drug shortages were for generic sterile injectables, which are critical but poorly compensated.
How long do drug shortages usually last?
The average drug shortage in 2022 lasted nearly 10 months-up from just over 6 months in 2015. Oncology drugs had the longest duration, averaging 14.3 months. Some shortages last years, especially if they involve a single manufacturer with a quality issue that takes time to fix. Even after a drug returns to market, it can take weeks or months for hospitals to restock and resume normal use.
Can I get a shortage drug from another country?
No. Importing medications from other countries is illegal in the U.S. unless done through FDA-approved channels, which are not available for individual patients. Even if a drug is available in Canada or India, bringing it in personally violates federal law. Some patients try online pharmacies, but many are unregulated and sell counterfeit or expired products. The safest option is to work with your pharmacist and doctor to find an approved alternative.
Do insurance companies cover drug alternatives?
Sometimes, but not always. Insurance plans often have formularies that only cover specific drugs. If your medication is in shortage and your doctor prescribes a substitute, your insurer may deny coverage if the alternative isn’t on their approved list. Always check with your pharmacy or insurer before switching. In many cases, your provider can file a prior authorization request, but that can take days or weeks.
Is there a way to predict when a drug will go into shortage?
Yes-but only if you’re connected to the right systems. The FDA maintains a public Drug Shortage Database, but it only lists drugs after the shortage has been officially reported. Hospitals with advanced monitoring tools can detect early warning signs: delayed shipments, reduced order quantities, or supplier communications. Some pharmacy networks use AI-driven analytics to flag anomalies before the FDA updates its list. Proactive hospitals that monitor these signals can prepare weeks in advance, reducing the impact on patients.

