Every year, over 1.3 million people in the U.S. end up in the emergency room because of problems with their medications. Many of these cases aren’t accidents-they’re preventable. Taking a prescription drug doesn’t mean you’re safe just because a doctor wrote the script. The truth is, medication errors happen more often than most people realize, and the consequences can be serious-even deadly.
Why Medication Safety Isn’t Just the Doctor’s Job
You might think that once your doctor prescribes a drug and the pharmacist fills it, your part is done. But that’s not how it works. Medication safety is a team effort. And you’re a key player. The World Health Organization calls this the Medication Without Harm challenge, and it’s not just a slogan. It’s a global effort to cut preventable harm by half. That means your actions matter.Think about it: you’re the one who takes the pill. You’re the one who notices if something feels off. You’re the one who remembers what else you’re taking. No algorithm or nurse can replace that.
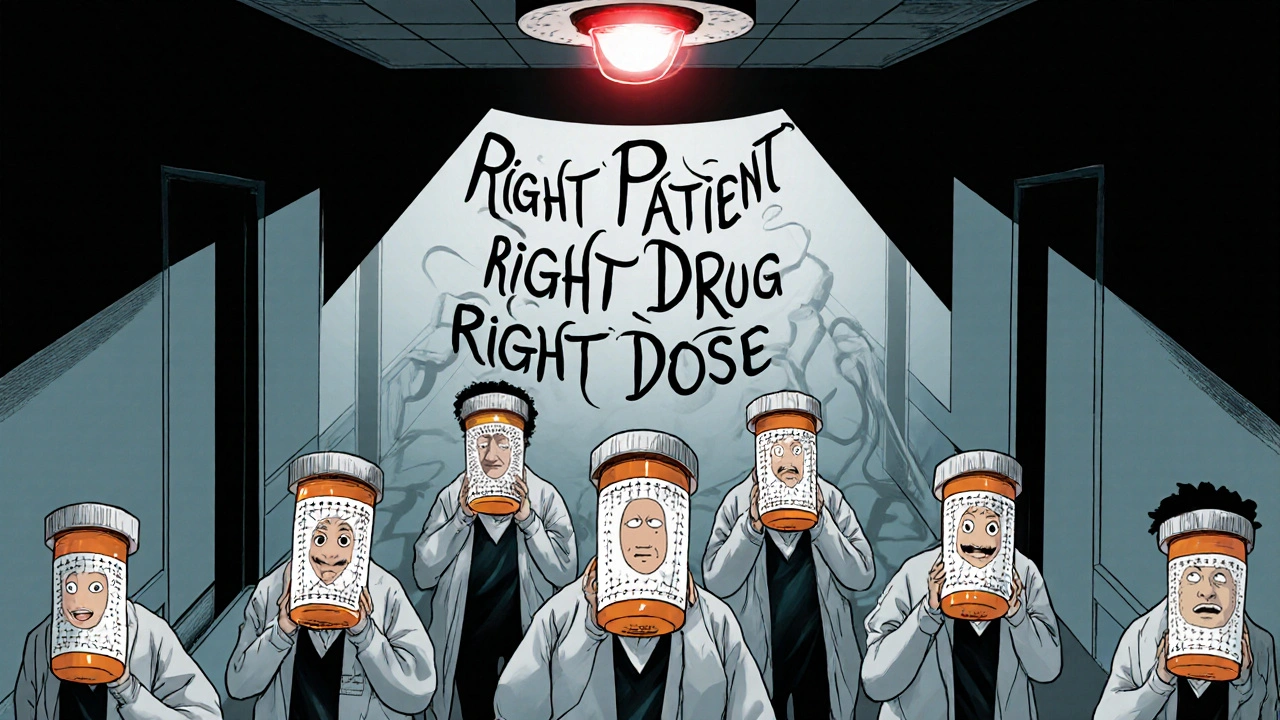
The 5 Rights of Safe Medication Use
Healthcare professionals use the 5 Rights to avoid mistakes:- Right patient - Is this medicine really for you? Double-check your name on the bottle.
- Right drug - Does the name match what your doctor said? Look for look-alike names like glimepiride and glyburide-both treat diabetes, but mixing them can crash your blood sugar.
- Right dose - Is it 5 mg or 50 mg? A tenfold mistake is common with insulin or blood thinners.
- Right route - Is it meant to be swallowed, injected, or applied to the skin? Taking a patch orally can be fatal.
- Right time - Are you taking it with food? At night? Every 8 hours? Timing affects how well it works and how safe it is.
Even if you’re not a nurse, use these five checks every time you take a pill. It’s that simple. And that powerful.
Know Your Medications-Don’t Guess
The CDC found that 63% of adults can’t correctly name all their medications or say why they’re taking them. That’s terrifying. If you don’t know what’s in your medicine cabinet, you’re playing Russian roulette with your health.Start with a simple list. Write down:
- The brand and generic name of each drug
- The dose and how often you take it
- Why your doctor prescribed it
- Any side effects you’ve noticed
- Supplements, vitamins, or over-the-counter drugs you use
Keep this list on your phone and carry a printed copy to every appointment. Bring it to the ER if you’re ever admitted. Half of all medication errors happen during care transitions-when you move from hospital to home, or from one doctor to another. Your list can stop that.
Ask the 8 Questions the FDA Wants You To
When you get a new prescription, don’t just walk out with the bottle. Ask your doctor or pharmacist:- What’s the name of this medicine?
- What’s the active ingredient?
- Why am I taking it?
- How much should I take, and when?
- What does it look like? (So you know if a refill looks different.)
- When does it expire?
- What side effects should I watch for?
- What should I avoid while taking it? (Alcohol? Other meds? Certain foods?)
- What if I miss a dose?
Don’t be shy. This isn’t bothering them-it’s helping them. A 2021 study in JAMA Network Open found that patients who were asked to repeat instructions back in their own words (called the “teach-back” method) were 40% more likely to take their meds correctly.

Watch Out for High-Risk Drugs
Some medications are more dangerous than others. These are called high-alert medications, and they include:- Insulin
- Warfarin (a blood thinner)
- Heparin (another blood thinner)
- Intravenous oxytocin (used in labor)
These drugs are responsible for about 30% of all serious medication errors, according to the American Society of Health-System Pharmacists. A tiny mistake with insulin can send someone into a coma. A wrong dose of warfarin can cause a stroke or uncontrolled bleeding.
If you’re on one of these, be extra careful. Use a pill organizer. Set phone alarms. Ask your pharmacist to explain the risks again. And never, ever change your dose without talking to your provider.
Don’t Rely on Memory-Use Tools
If you take more than two or three medications, your brain can’t keep track. That’s normal. You don’t need to be a genius to manage your meds-you need the right tools.- Pill organizers - Studies show they reduce errors by 35% in older adults.
- Smartphone reminders - Set alarms for each dose. Label them clearly: “Morning Blood Pressure Pill.”
- Barcode scanning apps - Some pharmacies offer apps that scan your pill bottle and give you a video explanation of how to take it.
- Medication safety apps - The CDC launched a free app in January 2024 called the “Medication Safety Checklist.” It helps you track your meds, set alerts, and even flag dangerous interactions.
One Reddit user shared how they accidentally took the wrong diabetes pill for three days because glimepiride and glyburide looked identical. Their blood sugar crashed. They ended up in the ER. A pill organizer with labeled compartments could’ve prevented that.
Never Stop or Skip Without Talking to Your Doctor
It’s common to feel better and think, “I don’t need this anymore.” But stopping antibiotics early is one of the biggest mistakes people make. The FDA says 23% of antibiotic treatment failures happen because people quit too soon.Same goes for blood pressure pills, antidepressants, or thyroid meds. Stopping suddenly can cause rebound effects-your symptoms come back worse. Always talk to your provider first. They might need to taper you off slowly.
Clean Out Your Medicine Cabinet Twice a Year
Expired meds aren’t just useless-they’re dangerous. The Illinois Department of Public Health found that 38% of accidental poisonings in children happen because of old pills left in cabinets.Do a medicine cabinet clean-out every spring and fall. Throw away:
- Drugs past their expiration date
- Anything that’s changed color, texture, or smell
- Unused antibiotics or painkillers
Don’t flush them down the toilet or toss them in the trash. Many pharmacies have take-back bins. Or check with your local police station-they often collect old meds for safe disposal.
Pharmacists Are Your Secret Weapon
Most people think pharmacists just hand out pills. They’re wrong. Pharmacists are medication experts. They know interactions, side effects, and how to spot dangerous combinations.Studies show that patients who ask their pharmacist about a new prescription have 27% fewer errors. Walk up to the counter and say: “I just got this new medicine. Can you tell me what to watch out for?”
They’re trained to answer. And they’ll appreciate you for asking.
What Happens When Safety Falls Through the Cracks?
Medication errors cost the U.S. healthcare system $42 billion a year. That’s 5% of all healthcare spending. But behind that number are real people:- A 72-year-old woman who took two blood pressure pills because she forgot she already took one.
- A teenager who mixed alcohol with his anxiety meds and ended up in intensive care.
- An elderly man who kept an old insulin pen after switching brands and accidentally injected the wrong dose.
These aren’t rare. They’re common. And they’re preventable.
Start Today: 3 Simple Steps to Safer Medication Use
You don’t need a PhD to stay safe. Just three actions:- Make or update your medication list today. Include everything-even ginseng and fish oil.
- Ask your pharmacist the 8 FDA questions the next time you pick up a prescription.
- Set a phone reminder for your next medicine cabinet clean-out-two months from now.
Medication safety isn’t about perfection. It’s about awareness. It’s about asking questions. It’s about not assuming. It’s about being the best advocate for your own body.
Because when it comes to your health, no one else will do it for you.
What should I do if I think I took the wrong pill?
Don’t wait. Call your pharmacist or poison control at 1-800-222-1222 right away. If you’re having symptoms like dizziness, trouble breathing, chest pain, or confusion, go to the ER. Bring the pill bottle with you-even if it’s empty. The label helps them identify what you took.
Can I split or crush my pills to make them easier to take?
Only if your doctor or pharmacist says it’s safe. Many pills are designed to release slowly-crushing them can cause a dangerous overdose. Extended-release pills, capsules with beads, and coated tablets should never be split or crushed. Always ask before changing how you take a medicine.
Why do some pills look different when I refill them?
That’s normal. Different manufacturers make the same generic drug, so color, shape, or size can change. But the name and dose should stay the same. Always check the label for the drug name and strength. If you’re unsure, call your pharmacy. Never assume it’s the same pill just because it treats the same condition.
Is it safe to take leftover antibiotics for a new infection?
No. Antibiotics are specific to the type of infection. Taking the wrong one can make the infection worse or cause dangerous side effects. Also, leftover antibiotics are likely expired or incomplete in dosage. Never use old prescriptions-even if you had the same illness before. Always get a new prescription.
How do I know if my medication is interacting with something else?
Tell every doctor and pharmacist about everything you take-prescription, over-the-counter, vitamins, supplements, and even herbal teas. Some interactions are serious: grapefruit can make cholesterol meds toxic. St. John’s wort can cancel out antidepressants. Use the CDC’s free Medication Safety Checklist app to scan for possible interactions. When in doubt, ask.


Kihya Beitz
November 15, 2025 AT 14:48Wow. Another ‘take your meds or die’ lecture. I’m sure the 1.3 million ER visits are just because people didn’t read this exact post. 🙄 I’ve been on 7 meds since I was 22. I don’t need a textbook to tell me to check the label. My pharmacist knows my name. My dog knows my schedule. Chill out.
Jennifer Walton
November 15, 2025 AT 23:24Responsibility is a social construct. The system designs pills to look alike, labels to blur, and instructions to confuse. We’re not failing the system. The system is failing us.
Adam Dille
November 17, 2025 AT 23:20This is actually super helpful 😊 I just started on blood pressure meds and was totally clueless. Made my list today and set alarms for 8am and 8pm. Also asked my pharmacist about the grapefruit thing-turns out I’m lucky I didn’t eat half a dozen last week. Thanks for the nudge!
Katie Baker
November 18, 2025 AT 21:10I love how you included the CDC app! I’ve been using it for two months now and it’s a game-changer. Even my mom (who hates tech) started using it after I showed her. So glad we’re making this stuff more accessible 💪
John Foster
November 19, 2025 AT 22:06Medication safety is not about individual diligence. It’s about the erosion of institutional accountability. The pharmaceutical industry thrives on complexity. The FDA is captured. Pharmacists are overworked. Doctors are incentivized to prescribe, not educate. The 5 Rights? A Band-Aid on a hemorrhage. We’ve turned human health into a compliance checklist while the real rot festers in corporate boardrooms and patent filings. You can’t ‘safety’ your way out of a system designed to profit from your ignorance.
Edward Ward
November 21, 2025 AT 13:01Can we talk about how the ‘8 FDA questions’ are great in theory, but in practice, most doctors are rushing through 20 patients an hour? I asked my doc about my new anticoagulant-she said, ‘Just take it daily,’ and walked out. Meanwhile, the pharmacist had to explain the interaction with my turmeric supplement, the timing with food, the INR target range, the signs of bleeding, the alcohol warning, the travel considerations, and the fact that my insurance only covers the generic, which looks nothing like the brand. So yes, the 8 questions are essential-but the system doesn’t give you the time to ask them. That’s the real problem.
Andrew Eppich
November 21, 2025 AT 22:20It is unacceptable that citizens must bear the burden of medical literacy. The responsibility for safe pharmaceutical administration lies with licensed professionals. To suggest that laypersons should memorize drug names, dosages, and interactions is to abdicate professional duty. This post, while well-intentioned, promotes dangerous individualism in a field that demands systemic oversight.
Jessica Chambers
November 22, 2025 AT 23:33My grandma died because she took two different blood thinners at the same time. The pharmacy didn’t flag it. The doctor didn’t ask. The hospital didn’t check. So yeah, I make a list. I take pictures of every pill. I set 12 alarms. And I still don’t trust anyone. 😒
Shyamal Spadoni
November 23, 2025 AT 20:08you know what this is really about? the cia and big pharma are working together to make us dependent on pills so they can control the population. the 5 rights? fake. the app? tracking. the pill organizers? microchips. they want you to think you’re safe but you’re just being programmed. i saw a guy on youtube who said his insulin pen vibrated before he took it-thats not a feature, its a signal. theyre watching. dont fall for it. also i think my neighbor is a robot
Ogonna Igbo
November 24, 2025 AT 22:55Why do Americans always think they need to write 2000 words to explain something simple? In Nigeria, we just ask the pharmacist and take the pill. No apps. No lists. No alarms. We have more respect for medicine than you do. You treat pills like toys. We treat them like weapons. That’s why our death rates are lower. You overthink. We just know. Stop making everything so complicated.