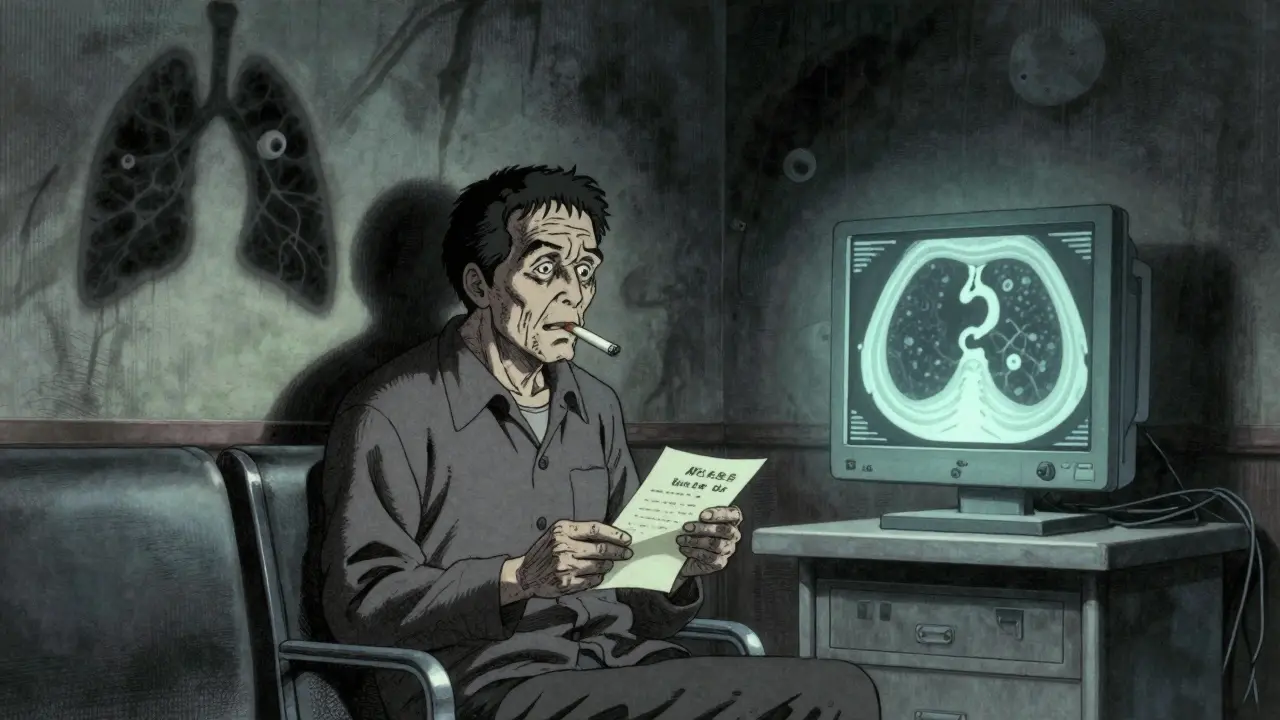
Every year, more people die from lung cancer than from colon, breast, and prostate cancers combined. And yet, most of those deaths could have been prevented-if the cancer had been caught early. For smokers and former smokers, there’s now a real chance to change that outcome. The tools are here: low-dose CT scans for early detection and targeted drugs that attack cancer at its genetic roots. But knowing about them isn’t enough. The real challenge is getting the right people screened, and then using what we find to guide treatment before it’s too late.
Who Should Be Screened? It’s Not Just Long-Time Smokers Anymore
For years, lung cancer screening was only recommended for people who smoked at least 30 pack-years and were between 55 and 80. A pack-year means smoking one pack a day for a year. So 30 pack-years could be one pack a day for 30 years, or two packs a day for 15 years. But in 2023, the American Cancer Society updated its guidelines to include anyone aged 50 to 80 with a 20-pack-year history-even if they quit smoking more than 15 years ago. That’s a big shift.Why? Because research shows the risk doesn’t disappear after quitting. A 2022 study in JAMA Oncology found that people who quit smoking 15 to 30 years ago still had 2.5 times the risk of lung cancer compared to people who never smoked. That means a 65-year-old who quit in 2005 is still at serious risk. The old rule-screen only if you quit within the last 15 years-left millions unprotected.
Medicare now covers screening for people aged 50 to 77 with a 20-pack-year history who currently smoke or quit within the past 15 years. But not all insurers follow this. Some still require 30 pack-years or only screen people aged 55 and up. That creates confusion. If you’re a former smoker who quit 20 years ago and are now 60, you might be eligible under the latest guidelines but denied coverage. Always ask your doctor. Don’t assume.
How Screening Works: The LDCT Scan
The only proven method for early detection is a low-dose CT scan, or LDCT. It’s not a chest X-ray. It’s a quick, painless scan that takes detailed images of your lungs using far less radiation than a regular CT. A typical LDCT uses 70-80% less radiation than a standard diagnostic scan. You lie on a table, hold your breath for a few seconds, and it’s done. No needles. No fasting. No recovery time.The goal? Find tumors before they spread. When lung cancer is caught early-before it leaves the lung-the five-year survival rate jumps to 59%. When it’s found late, after spreading to other organs, that number drops to just 6%. That’s the difference between a high chance of survival and a grim prognosis.
But here’s the catch: LDCT scans often show abnormalities that aren’t cancer. In fact, the National Lung Screening Trial found that 96.4% of positive scans turned out to be false alarms. That means for every 100 people flagged as having a possible tumor, 96 don’t have cancer. Those false positives lead to more scans, biopsies, and anxiety. That’s why screening isn’t for everyone. If you have severe heart disease, advanced COPD, or other conditions that make surgery or treatment risky, screening might not help you. It could even cause more harm.
Why So Few People Are Getting Screened
About 14.5 million Americans qualify for screening under the latest guidelines. But in 2021, only 2.6 million-just 18%-actually got screened. Why?First, many primary care doctors don’t know the updated guidelines. A 2022 AMA survey found 42% of them weren’t aware the age and pack-year requirements had been lowered. If your doctor doesn’t bring it up, you might never hear about it.
Second, access is uneven. Only 2,800 facilities in the U.S. are accredited by the American College of Radiology to perform screening. Rural areas have 67% fewer of these centers than cities. If you live outside a major metro area, you might have to drive hours just to get a scan.
Third, there’s stigma. Some people still think lung cancer is “their fault” because they smoked. That shame stops them from seeking help. But screening isn’t about blame-it’s about survival. Even if you smoked for decades, catching cancer early gives you a real shot at beating it.
And then there’s the gap in racial equity. Black individuals eligible for screening are 35% less likely to get screened than white individuals. That’s not a coincidence. It’s a system failure.
Targeted Therapy: When Screening Finds a Tumor
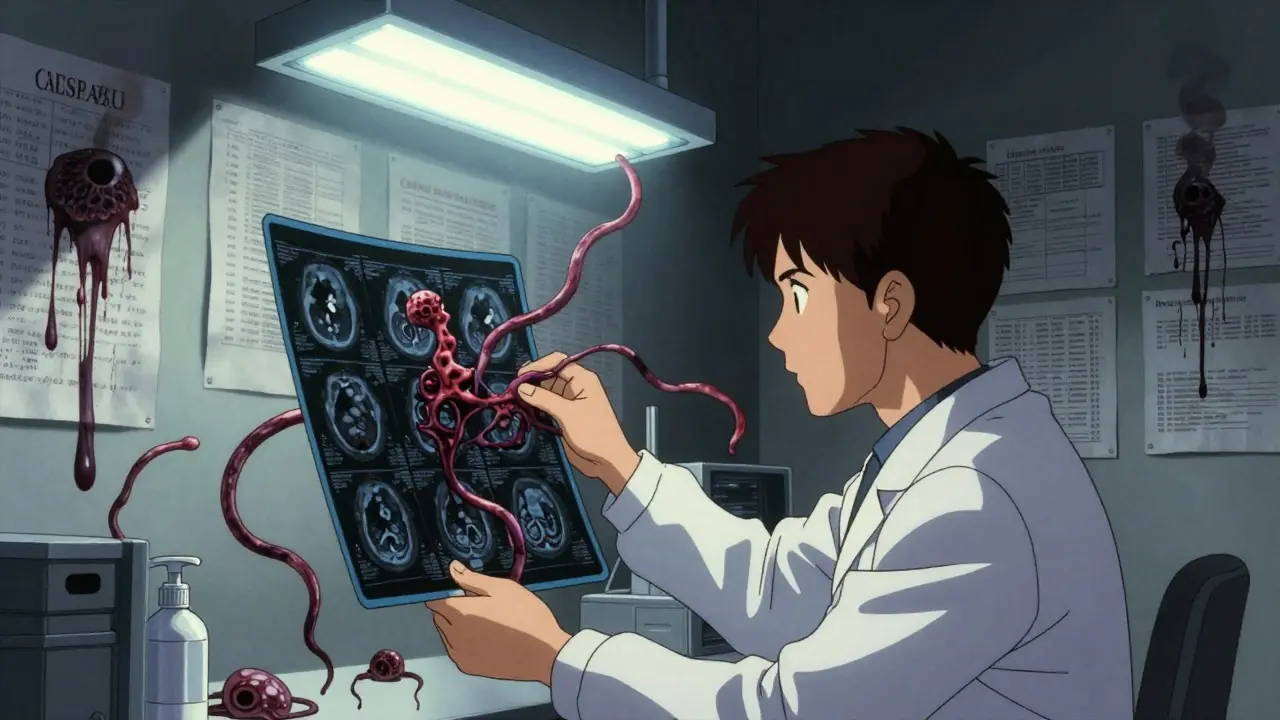
Finding a tumor early is only half the battle. What you do next matters just as much. That’s where targeted therapy comes in.Not all lung cancers are the same. About 15-20% of non-small cell lung cancers have a mutation in the EGFR gene. Another 3-7% have an ALK rearrangement. These aren’t random-they’re specific changes in the cancer’s DNA that drive its growth. And there are drugs designed to block them.
The drug osimertinib, approved in 2020 for early-stage EGFR-positive lung cancer, changed the game. In the ADAURA trial, patients who had surgery and then took osimertinib had an 83% reduction in the risk of cancer returning. That’s not just longer life. That’s a near-complete prevention of recurrence.
But here’s the key: you need to know if your tumor has these mutations. That’s why screening is so powerful. When you catch cancer early, there’s usually enough tissue from the biopsy to run genetic tests. In late-stage disease, tumors are often too spread out or too damaged to test properly. Early detection means more patients can benefit from these drugs.
By 2025, experts predict that 70% of early-stage lung cancers found through screening will have an actionable genetic mutation. That’s up from just 30% in late-stage cases. That’s the power of catching it early.
The Future: AI, Blood Tests, and Personalized Risk
The next wave of progress isn’t just about better scans or drugs-it’s about smarter screening.Artificial intelligence is already helping. The FDA approved LungQ by Riverain Technologies in January 2023. This software analyzes LDCT scans and flags suspicious nodules more accurately. In trials, it cut unnecessary follow-up scans by 22%. That means fewer false alarms, less anxiety, and lower costs.
But the real frontier is liquid biopsy. Instead of waiting for a tumor to show up on a scan, researchers are testing blood for tiny fragments of cancer DNA. If they can detect lung cancer before it’s visible on a CT scan, screening could shift from “detecting tumors” to “catching cancer before it forms.” Clinical trials like NCT04541082 are already testing this. It’s not ready for prime time yet, but it’s coming.
And then there’s personalized risk scoring. The National Cancer Institute is running the PACIFIC trial, launching in 2024. It’s testing whether combining smoking history with genetic markers, air pollution exposure, and family history can predict who’s at highest risk. That could mean screening only the people who need it most-reducing false positives and saving resources.
What You Can Do Right Now
If you’re a current or former smoker aged 50 or older with a 20-pack-year history:- Ask your doctor about lung cancer screening. Don’t wait for them to bring it up.
- Confirm your screening center is accredited by the American College of Radiology.
- Request a shared decision-making visit. This is a 15-minute conversation where your doctor explains risks and benefits. It’s required for Medicare coverage and helps you make an informed choice.
- If you’re still smoking, ask about quitting programs. Screening doesn’t replace quitting-it complements it. Nearly 70% of screened smokers want to quit, but only 30% get help.
- After a scan, follow up. If a nodule is found, stick with the recommended timeline for repeat scans. Don’t ignore it.
Screening saves lives. But only if you use it. The technology, the guidelines, the drugs-they’re all here. What’s missing is action.
Who qualifies for lung cancer screening?
You qualify if you’re between 50 and 80 years old, have a 20-pack-year smoking history (for example, one pack a day for 20 years), and currently smoke or quit within the past 15 years. The American Cancer Society’s 2023 guidelines also include former smokers who quit more than 15 years ago, as long as they’re still in the 50-80 age range. Always check with your insurance provider, as coverage rules vary.
Is the LDCT scan dangerous because of radiation?
No, not when done properly. A low-dose CT scan uses 70-80% less radiation than a standard diagnostic CT. The amount is similar to what you’d get from natural background radiation over about six months. The risk from radiation is far lower than the risk of missing an early-stage lung cancer. Annual screening is considered safe for eligible individuals.
What if the scan finds a nodule? Does that mean I have cancer?
Not at all. Most nodules found on LDCT scans are not cancer. In fact, over 96% of positive scans turn out to be false positives. A nodule could be scar tissue, an infection, or a harmless growth. The next step is usually a follow-up scan in 3-6 months to see if it grows. Only if it changes size or shape will doctors consider a biopsy. Don’t panic-follow your doctor’s advice.
Can targeted therapy cure lung cancer?
It’s not a cure, but it can dramatically improve outcomes. For patients with specific gene mutations like EGFR or ALK, drugs like osimertinib can reduce the risk of cancer returning after surgery by 83%. These drugs don’t eliminate all cancer cells, but they keep the disease under control for years. They’re most effective when used early, which is why screening is so important.
Why are screening rates so low among Black and rural populations?
Systemic barriers. Rural areas have far fewer accredited screening centers. Black patients are less likely to be offered screening, even when eligible, due to provider bias and lack of outreach. Insurance coverage gaps and mistrust in the medical system also play a role. Addressing this requires targeted outreach, mobile screening units, community health workers, and better provider education.
Next Steps if You’re at Risk
If you’re unsure whether you qualify, calculate your pack-years: multiply the number of packs you smoked per day by the number of years you smoked. If it’s 20 or more, and you’re 50 or older, schedule a talk with your doctor. Bring the American Cancer Society’s 2023 guidelines with you. Ask if you’re eligible for screening. Ask if your insurance covers it. Ask about quitting resources-even if you quit years ago, your lungs still need support.Early detection and targeted therapy are no longer theoretical. They’re here. And they’re working. The question isn’t whether these tools exist. It’s whether you’ll use them.