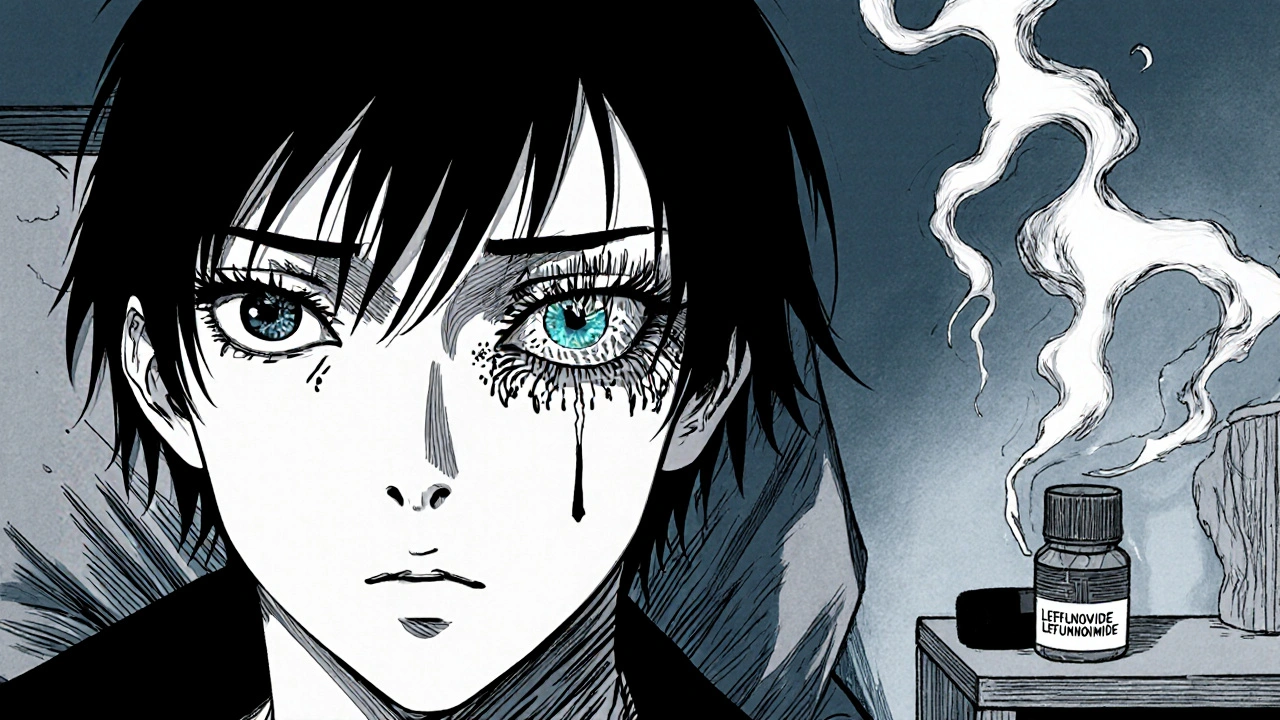
When you’re on Leflunomide is a disease‑modifying antirheumatic drug (DMARD) used for rheumatoid arthritis and other autoimmune conditions. While it’s effective at slowing joint damage, a small but real risk of eye problems can catch patients off guard.
Key Takeaways
- Eye‑related side effects from leflunomide are rare (<1% of users) but can be serious.
- Typical symptoms include blurred vision, dry eye, uveitis, and, in extreme cases, optic neuritis.
- Immediate ophthalmology referral is essential if any visual change occurs.
- Regular eye checks are recommended for high‑risk patients (e.g., those with prior eye disease).
- Alternative DMARDs such as methotrexate or sulfasalazine have different eye‑risk profiles.
How Leflunomide Works
Leflunomide blocks the enzyme dihydroorotate dehydrogenase, which reduces synthesis of pyrimidine nucleotides. This limits the proliferation of activated T‑cells, the culprits behind joint inflammation. Because the drug interferes with DNA synthesis, it can also affect rapidly renewing cells in the eye’s surface and retina, which explains the occasional ocular side effects.
Common Systemic Side Effects
Before diving into eye issues, it helps to remember the more frequent problems:
- Gastrointestinal upset (nausea, diarrhea)
- Elevated liver enzymes
- Hair thinning
- Hypertension in a minority of users
These systemic signs often prompt clinicians to order regular blood tests, but eye monitoring can be overlooked.

Eye‑Related Adverse Events Linked to Leflunomide
Published post‑marketing data and case series (e.g., a 2023 European pharmacovigilance report) identify several ocular manifestations:
- Dry eye syndrome - reported in roughly 0.4% of patients, characterized by gritty sensation and intermittent blurred vision.
- Uveitis - inflammation of the uveal tract; incidence around 0.1% but can threaten vision if untreated.
- Optic neuritis - rare (<0.05%) inflammatory demyelination of the optic nerve, leading to sudden vision loss.
- Retinal toxicity - isolated case reports describing pigmentary changes and reduced visual fields.
Most of these events appear within the first six months of therapy, though delayed onset up to two years has been documented.
Recognizing Early Symptoms
Prompt detection hinges on patients knowing what to look for. Typical red flags include:
- Persistent gritty or burning feeling despite artificial tears
- New floaters, flashes, or a curtain‑like shadow in peripheral vision
- Sudden loss of color contrast or blurred central vision
- Painful eye movement, especially with light exposure
If any of these arise, stop the drug only after a clinician’s advice and arrange an urgent appointment with an Ophthalmologist.
Managing Eye Problems While on Leflunomide
Management strategies differ by the specific condition:
- Dry eye syndrome: lubricating eye drops (preservative‑free), punctal plugs for refractory cases, and consider dose reduction if symptoms persist.
- Uveitis: topical steroids are first‑line; systemic steroids or immunosuppressants may be needed for posterior involvement. Many clinicians opt to switch from leflunomide to an alternative DMARD.
- Optic neuritis: high‑dose intravenous methylprednisolone followed by oral taper, immediate discontinuation of leflunomide, and MRI to rule out demyelinating disease.
- Retinal toxicity: discontinue leflunomide, perform optical coherence tomography (OCT) to assess retinal layers, and refer to a retinal specialist.
Throughout, keep the FDA briefing documents in mind - they advise that any ocular event demanding treatment should trigger drug cessation and a risk‑benefit reassessment.
Comparing Eye‑Risk Profiles of Common DMARDs
| Drug | Incidence of Dry Eye | Uveitis Cases | Optic Neuritis Reports | Monitoring Recommendation |
|---|---|---|---|---|
| Leflunomide | 0.4 % | 0.1 % | 0.05 % | Baseline eye exam, then every 6 months if symptomatic |
| Methotrexate | 0.1 % | Rare | Very rare | Routine exam only if ocular symptoms develop |
| Sulfasalazine | 0.2 % | 0.05 % | 0.01 % | Annual eye check recommended |
Notice that leflunomide carries a slightly higher risk for dry eye and uveitis compared to methotrexate, while sulfasalazine falls in the middle. This information helps clinicians choose the safest option for patients with pre‑existing eye disease.
Practical Monitoring Guidelines
Here’s a checklist you can share with patients:
- Baseline comprehensive eye exam before starting leflunomide.
- Educate about red‑flag symptoms (list from earlier section).
- Schedule follow‑up eye visits at 3 months and 6 months, then annually if no issues.
- Coordinate with the rheumatology team to adjust dosage or switch therapy when needed.
- Document any ocular event in the medication safety record per American Academy of Ophthalmology guidelines.
Frequently Asked Questions
Can leflunomide cause permanent vision loss?
Permanent loss is exceedingly rare. Most reported cases, such as dry eye or mild uveitis, resolve with prompt treatment. Optic neuritis can lead to lasting deficits if therapy is delayed, so early ophthalmic evaluation is critical.
Do I need an eye exam before every prescription refill?
Not for every refill. A baseline exam plus a check at three months, then every six months if symptoms appear, satisfies most safety recommendations.
Is it safe to use over‑the‑counter eye drops while on leflunomide?
Preservative‑free artificial tears are generally safe and can relieve dryness. Avoid drops containing steroids unless prescribed by an ophthalmologist.
Should I stop leflunomide if I develop mild dry eye?
Mild cases usually respond to lubricants and dose adjustment rather than outright discontinuation. Discuss any change with your rheumatologist first.
Are there any vaccines that interact with leflunomide and eye health?
Live vaccines are generally avoided while on leflunomide because of immunosuppression, but they do not directly affect the eye. Inactivated vaccines are safe.
Understanding the eye‑related risks of leflunomide empowers patients and clinicians to catch problems early, keep vision clear, and stay on effective arthritis therapy.

Mary Mundane
October 24, 2025 AT 15:29Honestly, if you’re not getting any vision issues, stop obsessing over a myth.
Michelle Capes
November 4, 2025 AT 00:29I get how scary it can feel when a drug mentions eye risks 😟. Even if it’s rare, keep an eye on any blurry vision or pain, and let your doc know right away. It’s better to be safe than sorry.
Dahmir Dennis
November 14, 2025 AT 10:29Oh great, another “rare” side effect that nobody talks about until you’re staring at the ceiling because your eyes feel like sandpaper. Yeah, because the pharma companies love to bury the stuff that could actually ruin your day. If you’re on leflunomide and suddenly see spots, maybe it’s the medication, maybe it’s just your imagination-but hey, why not blame the drug? The real tragedy is that most patients never even hear about this until it’s too late. So, kudos to the guide for finally spilling the beans.
Jacqueline Galvan
November 24, 2025 AT 20:29Patients prescribed leflunomide should be aware that ocular adverse events, although uncommon, have been documented in clinical trials.
The most frequently reported eye‑related issues include dry eye syndrome and transient visual disturbances.
Less commonly, patients may experience optic neuritis, uveitis, or retinal toxicity, each of which warrants immediate medical attention.
It is essential to schedule regular ophthalmologic examinations prior to initiating therapy and at periodic intervals thereafter.
Baseline assessments should include visual acuity testing, intraocular pressure measurement, and a thorough slit‑lamp examination.
Should any new ocular symptoms arise-such as blurred vision, eye pain, or photophobia-the prescribing physician must be notified without delay.
Prompt referral to an ophthalmologist can facilitate early detection and management, potentially averting irreversible damage.
Management strategies may involve temporary discontinuation of leflunomide, dosage adjustment, or adjunctive treatment with lubricating eye drops.
In cases of confirmed optic neuritis, high‑dose corticosteroids are often employed to reduce inflammation.
Patients with a history of autoimmune eye disease should discuss risks with their rheumatologist before starting leflunomide.
Documentation of any ocular side effect in the patient’s medical record aids future clinical decision‑making.
Recent pharmacovigilance data suggest that the incidence of serious eye complications remains below one percent across large patient populations.
Nevertheless, vigilance is prudent, as early intervention can markedly improve visual outcomes.
Education on symptom recognition empowers patients to act swiftly, fostering a collaborative approach to safety.
Ultimately, while leflunomide remains an effective disease‑modifying agent, integrating regular eye care into treatment plans optimizes both joint and visual health.
Tammy Watkins
December 5, 2025 AT 06:29While the preceding exposition delineates a commendable protocol, one must underscore the exigency of patient‑centric vigilance; indeed, the onus lies not solely upon the clinician but equally upon the individual to articulate any ocular perturbations with alacrity.
Dawn Bengel
December 15, 2025 AT 16:29Only a fool would ignore the fact that America’s drug regulators finally caught up with the rest of the world – leflunomide’s eye risks are real, and we’re proud to demand transparency! 🇺🇸👀
junior garcia
December 26, 2025 AT 02:29Yo, keep an eye out – literally. If it feels off, tell your doc.
Dason Avery
January 5, 2026 AT 12:29Indeed, the eye is a window to our soul; staying proactive preserves that view, and a quick check‑up can keep the world bright 🌟.
Casey Morris
January 15, 2026 AT 22:29Hey folks!!! I just wanted to chime in-remember, the eyes are the *mirrors* of our health, so don’t be lazy about reporting any weird sensations; early action = better outcomes!!!
Teya Arisa
January 26, 2026 AT 08:29It is indeed prudent to consider ophthalmic monitoring as an integral component of comprehensive care, and one might graciously affirm that such diligence reflects exemplary stewardship of patient welfare 😊.
Kester Strahan
February 5, 2026 AT 18:29Yo, the pharmaco‑kinetics of leflunomide show a lengthy half‑life, so accumulative ocular tox could creep up if you ain’t on the radar, ya feel me?
Doreen Collins
February 16, 2026 AT 04:29It’s essential to have regular eye exams while on leflunomide, and honestly, the risk is minimal, but you never know when a subtle change might indicate something bigger.
HILDA GONZALEZ SARAVIA
February 26, 2026 AT 14:29When you’re taking leflunomide, keep a personal log of any visual changes-whether it’s a slight blur, a flicker of light, or increased dryness. These subtle cues can be early flags. I’ve seen patients brush them off, only to later discover they needed a quick adjustment in therapy. Talk to your rheumatologist and get a baseline eye exam before you start the medication. If something feels off, schedule an ophthalmology visit promptly; it’s better to be safe than sorry. Even though serious eye complications are rare, the stakes are high when vision is involved. A proactive approach also eases anxiety because you know you’re covering all bases. Remember, your health team is there to help you navigate these nuances.