Every year, millions of people around the world take medicine they think is real-only to find out later it was fake. Counterfeit drugs don’t just waste money. They can kill. The World Health Organization says 1 in 10 medical products in low- and middle-income countries is substandard or falsified. Even in places with strong regulations, mistakes happen. That’s why knowing how to verify drug authenticity isn’t just a safety tip-it’s a necessity.
Why Drug Authenticity Matters
A counterfeit pill might look identical to the real thing. But instead of the active ingredient, it could have chalk, rat poison, or nothing at all. The FDA warns that fake medications may contain the wrong ingredients, incorrect dosages, or harmful contaminants. People taking fake antibiotics might not recover from infections. Fake cancer drugs can let tumors grow unchecked. And counterfeit heart medication? That’s a direct path to emergency rooms-or worse. The global market for fake pharmaceuticals is estimated at $200 billion annually. It’s not just happening in remote villages. Fake drugs show up in online pharmacies, travel destinations, and even legitimate-looking clinics. The only way to be sure you’re getting the real thing is to use verified tools and systems designed for this exact purpose.The EU Falsified Medicines Directive (FMD)
If you’re in Europe, the Falsified Medicines Directive (FMD) is your strongest defense. Implemented on February 9, 2019, it requires every prescription medicine package to have a unique 12-digit serial number, a tamper-evident seal, and a 2D barcode. When you pick up your medicine at the pharmacy, the pharmacist scans that barcode. The system checks it against the European Medicines Verification System (EMVS) in real time. If the code is valid and hasn’t been used before, the system confirms authenticity. If it’s already been scanned, duplicated, or blocked, the pharmacy gets an alert. This system is mandatory for all EU member states. A 2018 Delphi study found that 70% of NHS pharmacists rated the process as quick and user-friendly. The average verification time is just 3.2 seconds per package. The FMD system has one major advantage: it verifies the drug at the point of dispensing-right before it reaches you. That’s a critical layer of protection most other systems lack.The U.S. Drug Supply Chain Security Act (DSCSA)
In the United States, the DSCSA took effect in stages, with full implementation due by November 27, 2023. Unlike the EU, the U.S. system doesn’t require verification at the pharmacy counter. Instead, it focuses on tracking drugs as they move between manufacturers, distributors, and wholesalers. Each package gets a unique identifier, but it’s only checked when ownership changes-not when you get it from the pharmacist. This creates a gap. A fake drug could slip through if it enters the supply chain after the last verified handoff. That’s why the FDA proposed a rule in September 2023 to require patient-level verification by 2027. Until then, U.S. consumers don’t have the same direct verification access as Europeans. Some U.S. pharmacies have added their own scanning systems voluntarily. Independent pharmacies often use QR codes linked to manufacturer databases. But these aren’t standardized or required by law. That means if you’re in the U.S., you can’t assume your pharmacist is checking your medicine the same way a pharmacist in Germany or France does.Handheld Spectral Analyzers: Science in Your Hands
For healthcare workers in remote areas or countries without full serialization systems, handheld devices are changing the game. These tools use near-infrared (NIR) spectroscopy, Raman spectroscopy, or laser-induced fluorescence to scan a pill or vial and compare its spectral signature to a database of known authentic products. The technology isn’t new-but it’s getting better. In 2018, field accuracy was around 78%. By 2022, it jumped to 92%, according to USP testing data. Devices from Thermo Fisher Scientific and Agilent Technologies are now rugged enough for use in clinics, ambulances, and mobile health units. In Ghana, community health workers using these devices achieved 87% accuracy after 28 hours of training. That’s a big improvement over older methods like visual inspection or relying on packaging alone. The downside? These devices cost $2,000-$5,000 each. They’re not practical for most consumers-but they’re vital for frontline workers in places where fake drugs are common.
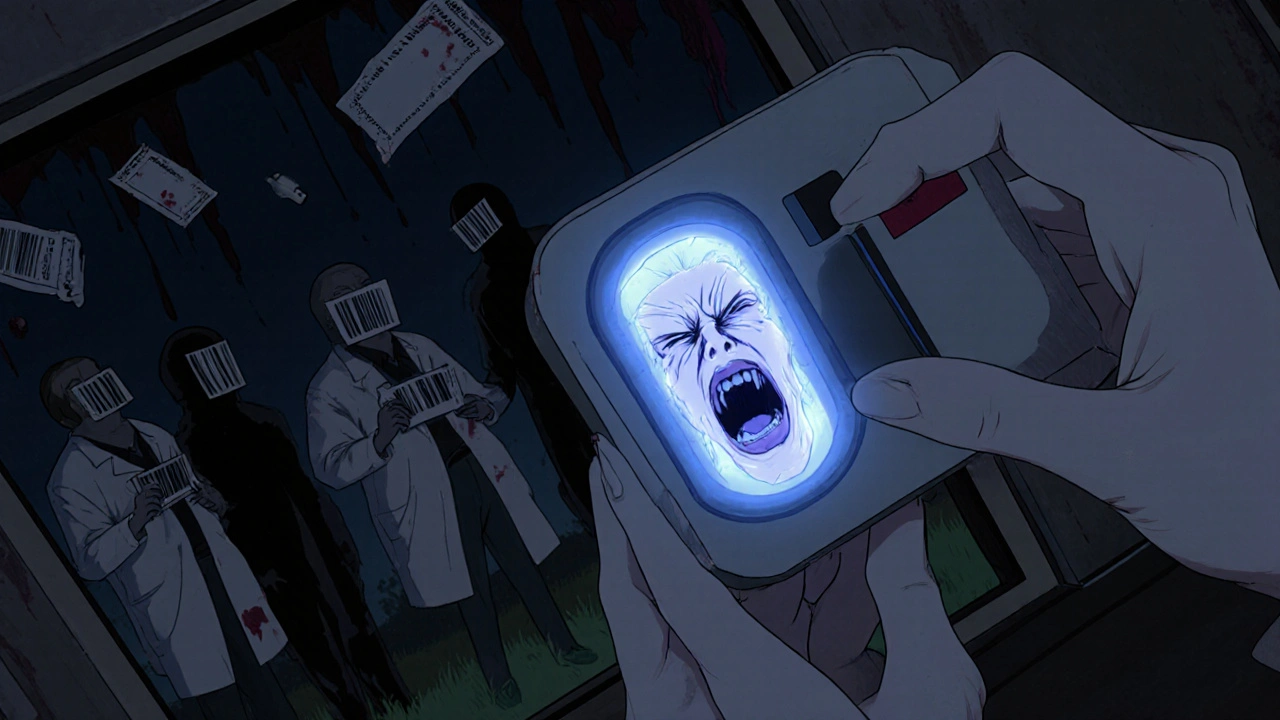
On-Dose Authentication: Invisible Markers
Some manufacturers are now putting invisible markers directly onto pills or capsules. These are called Physical Chemical Identifiers (PCIDs). They can be molecular taggants, special inks, or even DNA barcodes that are undetectable to the naked eye but readable with specialized scanners. Alveron Pharma is currently in Phase 3 trials with a DNA-based taggant system. It’s so precise it can identify a specific batch of medicine down to the production line. Accuracy rates hit 99.9%. The catch? It adds $0.03 to $0.15 per unit to manufacturing costs. That’s why it’s mostly used for high-value drugs like cancer treatments or insulin-not everyday painkillers. The FDA acknowledged these technologies in a January 2021 draft guidance but warned about regulatory hurdles. Adding chemicals to medicine-even harmless ones-requires extensive safety testing. So while promising, this method is still emerging.Blockchain and Digital Track-and-Trace
Blockchain is being tested by some of the biggest pharmaceutical companies. Pfizer, for example, has deployed blockchain-integrated serialization in 17 countries. The system logs every transfer of a drug package on a secure, tamper-proof digital ledger. Verification accuracy? 99.8%. The problem? It’s expensive. Implementing a blockchain system costs an average of $2.7 million per company. That’s why only 22% of the top 50 pharma firms have adopted it, according to Deloitte’s 2023 survey. Smaller companies can’t afford it. And patients still can’t scan it themselves. For now, blockchain is a back-end tool for supply chain security-not a consumer-facing solution. But it’s a key part of the future. As regulations tighten and costs drop, it could become the standard.What You Can Do as a Consumer
If you’re outside the EU, you don’t have a government-mandated verification system at your pharmacy. But you’re not powerless.- Check the packaging. Look for spelling errors, blurry printing, mismatched colors, or missing lot numbers. Fake drugs often have sloppy labeling.
- Buy from licensed pharmacies. Avoid online sellers that don’t require a prescription or won’t show a physical address. In the U.S., look for the VIPPS seal (Verified Internet Pharmacy Practice Sites).
- Compare the medicine. If your pill looks different from last time-color, shape, size, markings-ask your pharmacist. It might be a generic switch, but it might not.
- Use official apps. Some countries have apps that let you scan barcodes to check authenticity. India’s e-Sanjeevani and Kenya’s mPedigree are examples. These aren’t foolproof, but they’re better than nothing.
- Report suspicious drugs. If you suspect a fake, report it to your national health authority. In the U.S., use the FDA’s MedWatch program. In Australia, contact the TGA.
Common Pitfalls and How to Avoid Them
Even with technology, mistakes happen. Here are the most common issues:- Confusing alerts. In early FMD implementations, 43% of pharmacists mistook counterfeit warnings for “already dispensed” messages. Many pharmacies now use red for warnings and green for OK-making it clearer.
- System downtime. Pharmacies average 2.3 hours of system outages per month. If the scanner doesn’t work, the pharmacy should have a backup procedure-like manual lookup or holding the product until it’s verified.
- Expired drugs misidentified. Around 7.8% of verifications flag expired products as counterfeit. That’s because the system checks the serial code, not the expiration date. Always check the expiry date yourself.
- Human error. WHO says 72% of counterfeit detection failures are due to staff skipping steps or rushing. If you’re a patient, don’t assume the system caught everything. Stay involved.
The Future of Drug Verification
The future is moving toward integration. The FDA’s 2027 plan to add patient-level verification will close the biggest gap in the U.S. system. The European Medicines Agency is testing AI to spot anomalies in verification data-like sudden spikes in failed scans from one region, which could signal a counterfeit ring. The USP and FDA are also building a public spectral library. By 2025, it will include reference data for 1,200 essential medicines. That means future handheld devices will be able to compare your pill against an open, trusted database-not just proprietary ones. By 2030, McKinsey projects 95% global adoption of comprehensive authentication systems. But that won’t help anyone if the tools aren’t accessible. The real challenge isn’t technology-it’s equity. A blockchain system won’t save someone in rural Malawi if they don’t have internet or a smartphone. That’s why portable spectroscopy and low-cost QR codes are just as important as high-tech solutions.Final Takeaway
You can’t rely on luck or packaging alone. The safest way to verify drug authenticity is through official systems-FMD in Europe, licensed pharmacies everywhere, and handheld devices for professionals. As a consumer, your best tools are awareness, skepticism, and reporting. If something looks off, it probably is. Don’t take the risk. Ask questions. Demand transparency. Your life depends on it.How can I tell if my medicine is fake?
Look for signs like poor packaging quality, misspelled names, mismatched colors, or missing batch numbers. Compare the pill’s appearance to previous prescriptions. If it looks different, ask your pharmacist. In the EU, scan the 2D barcode at the pharmacy-it’s required by law. In other regions, buy only from licensed pharmacies and avoid online sellers without a physical address or prescription requirement.
Is the EU FMD system better than the U.S. DSCSA?
Yes, in terms of consumer protection. The EU FMD verifies every prescription drug at the point of dispensing-right before you get it. The U.S. DSCSA only requires verification when ownership changes between companies, not when you receive the drug. That means a fake drug could slip through in the U.S. if it enters the supply chain late. The FDA plans to fix this by 2027, but for now, the EU system offers stronger direct protection.
Can I use my phone to scan a medicine barcode?
In some countries, yes. Apps like mPedigree (Africa) and e-Sanjeevani (India) let you scan barcodes to check authenticity. In the EU, pharmacists use dedicated scanners linked to the national verification hub-your phone won’t work there. In the U.S., most systems aren’t consumer-accessible yet. Even if you scan a QR code, it only checks if the code is registered-not if the medicine inside is real. Always combine scanning with other checks.
Are handheld spectrometers available to the public?
Not currently. Devices that use NIR or Raman spectroscopy cost between $2,000 and $5,000 and require training to use correctly. They’re designed for healthcare workers in clinics, pharmacies, or field settings-not individual consumers. The technology is improving, but it’s not practical or affordable for personal use yet.
What should I do if I think I got a fake drug?
Stop taking it immediately. Contact your pharmacist or doctor. Report it to your country’s health authority-like the FDA’s MedWatch in the U.S., the TGA in Australia, or your national medicines agency. Keep the packaging and any receipts. If possible, take a photo. These reports help agencies track counterfeit networks and protect others.
Why don’t all countries have the same drug verification system?
It comes down to resources. The EU and U.S. have the infrastructure and funding to enforce complex systems like serialization and digital tracking. Many low-income countries lack reliable electricity, internet, or trained staff. Simpler methods like SMS verification or QR codes are used there-but they’re less reliable. Global efforts are underway to standardize systems, but progress is slow. Until then, access to safe medicine depends heavily on where you live.


Kevin Jones
November 19, 2025 AT 08:20EU FMD is a cryptographic triumph-real-time serialization at point-of-dispensing eliminates supply-chain ambiguity. The U.S. DSCSA? A fragmented, back-end ledger that fails at the final mile. Consumer protection isn't a feature-it's the endpoint, and America's system ignores it.
Erica Lundy
November 21, 2025 AT 01:02There is an ethical paradox here: we deploy technologies capable of verifying molecular authenticity at 99.9% precision, yet we deny access to those tools based on geography, income, or institutional capacity. The real crisis is not counterfeit drugs-it is the moral architecture that permits inequitable access to safety. If a child in Malawi dies from a fake antimalarial, is it a failure of supply-or of conscience?
Premanka Goswami
November 22, 2025 AT 02:04Let me tell you something they don’t want you to know-this whole verification system is a scam. The FDA and WHO are in cahoots with Big Pharma to keep you dependent. Those barcodes? They’re tracking chips. The ‘authentic’ pills are still laced with microchips to monitor your vitals. And the handheld spectrometers? They’re only sold to doctors who sign NDAs. You think they want you to verify your meds? No-they want you to trust them. Wake up.
Alexis Paredes Gallego
November 23, 2025 AT 23:19Oh wow, another ‘official tools’ article. Let me guess-next they’ll tell us to ‘trust the system’ while the same corporations that make the drugs also built the verification tech. The EU’s system? A PR stunt. The U.S. doesn’t even let you scan your own meds? That’s not oversight-that’s control. And don’t get me started on blockchain. It’s just corporate vanity wrapped in buzzwords. You’re being played.
Saket Sharma
November 25, 2025 AT 22:14PCID DNA taggants at $0.15/unit? Pathetic. Real pharma innovation requires CRISPR-tagged biomarkers with quantum-encrypted metadata. You’re still using barcodes? In 2025? The global supply chain demands blockchain-native, AI-audited, zero-trust verification. If your country can’t afford it, you’re not a patient-you’re collateral.
Shravan Jain
November 27, 2025 AT 00:37the eu fmd is just a glorified qr code system. and the us dscsa? lol. they dont even verify at the counter. why do you think so many fake pills are sold online? because the system is broken. also, the ‘spectrometers’? 5k? for what? to check if my tylenol is real? i’m not a scientist. this is all overengineered nonsense. and the ‘report it’ advice? good luck getting the fda to care.
Brandon Lowi
November 28, 2025 AT 16:51Let me get this straight: the EU-where they put ‘EU’ on everything-has a system that actually works. Meanwhile, America? Still letting pharmacists hand out pills like candy, with zero accountability. We’re the land of the free, but if you’re on insulin and get a fake vial? Too bad. We can’t afford to protect our own. This isn’t healthcare-it’s American Exceptionalism with a side of negligence.
Joshua Casella
November 30, 2025 AT 11:50I’ve worked in rural clinics where the only tool we had was a flashlight and a printed reference guide. The fact that we’re even talking about blockchain and DNA tags feels like a luxury. But here’s what matters: training. Empowering community health workers with simple, low-cost tools-like QR codes linked to open databases-is the real win. We don’t need perfection. We need access. And if we build it together, it’ll work for everyone-not just the wealthy.
Richard Couron
November 30, 2025 AT 15:37They say ‘scan the barcode’-but what if the barcode’s been cloned? What if the EMVS server is hacked? What if the pharmacist is paid off? You think this is about safety? It’s about control. The government doesn’t want you to verify your meds-they want you to believe they’ve verified them. And don’t get me started on the ‘official apps’-those are just Trojan horses for data harvesting. You’re being watched. Always.
Kevin Jones
November 30, 2025 AT 19:34And yet, the EU system has reduced counterfeit circulation by 62% in five years. That’s not theory-that’s data. The U.S. is still debating whether to let patients scan their own prescriptions. The difference isn’t technology. It’s political will. One region chose to protect lives. The other chose to protect profits.