Every morning, hundreds of thousands of children across the U.S. take their asthma inhalers, insulin shots, or ADHD meds right before homeroom. But who makes sure the right kid gets the right pill at the right time? It’s not the teacher. It’s not the principal. It’s the school nurse - and the system around them. Coordinating daily pediatric medications in schools isn’t just about handing out pills. It’s a high-stakes, legally binding process that can mean the difference between a child being safe at school or ending up in the ER.
Why School Nurses Are the Linchpin
School nurses don’t just treat scrapes and fevers. They’re the central hub for managing chronic conditions like diabetes, epilepsy, asthma, and severe allergies. According to the National Association of School Nurses (NASN), nearly 15% of all students need some form of daily medication during school hours. That’s one in seven kids. And if the nurse isn’t coordinating everything properly, mistakes happen. The data is clear: about 1.2% of all school-based medication administrations result in an error. That might sound small, but in a school of 1,000 students, that’s 12 mistakes a year - some life-threatening. The key to preventing those? A strong, consistent system led by the school nurse.The Five Rights: Non-Negotiable Rules
Every time a medication is given, the nurse must confirm the Five Rights:- Right student - Double-check name, date of birth, ID bracelet if used.
- Right medication - Match the label to the prescription.
- Right dose - Is it 5 mg or 50 mg? Don’t guess.
- Right route - Swallowed, inhaled, injected, or applied to skin?
- Right time - Within 30 minutes of the prescribed time, unless the doctor says otherwise.
Medication Containers: No Exceptions
Parents often bring meds in ziplock bags or old pill organizers. That’s a problem. Federal law (21 CFR § 1306.22) requires all medications administered in school to be in their original, pharmacy-labeled containers. That means the label must show:- Student’s full name
- Medication name and strength
- Dosage instructions
- Prescriber’s name
- Pharmacy name and phone number
Delegation: When Nurses Can’t Be Everywhere
The national average for school nurse-to-student ratio is 1:1,102. The recommended standard? 1:750 - and even that’s not enough for schools with complex medical needs. So nurses can’t be in every classroom at 10 a.m. for every pill. That’s where delegation comes in. Nurses can train trained unlicensed personnel (UAP) - like teachers, aides, or office staff - to give meds under strict rules. But here’s the catch: the nurse must assess both the student and the staff member first. - For simple oral meds (like ADHD pills), 4-8 hours of training is typical. - For insulin injections or seizure meds, training can be 12-16 hours. - Every first dose must be given by the nurse - no exceptions. Virginia’s model requires this, and their schools report 22% fewer adverse events than states without it. The nurse doesn’t just hand off the task - they verify competency, document training, and remain legally responsible.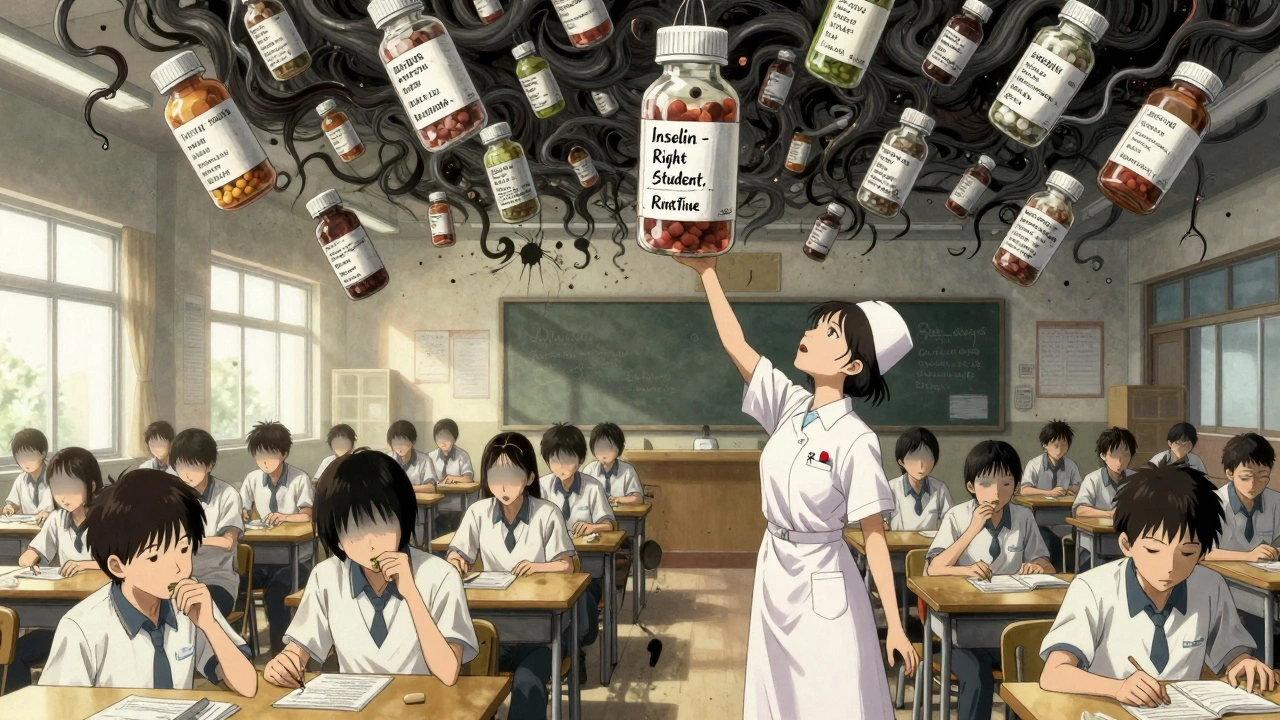
Documentation: The Paper Trail That Protects Everyone
Every time a medication is given, it must be recorded. Immediately. Not later. Not tomorrow. Right after. Most districts (98%) now use electronic health records (EHR), but 42 states still allow paper logs. The problem? Paper logs get lost, smudged, or forgotten. Fairfax County Public Schools switched to an EHR system and cut documentation time by 45% while improving accuracy by 31%. What to record:- Time and date given
- Medication and dose
- Who gave it
- Student’s response (e.g., nausea, drowsiness, no reaction)
- Any refusal or missed dose
Individualized Healthcare Plans (IHPs): The Blueprint for Safety
Not all kids are the same. A child with type 1 diabetes needs a detailed plan - when to check blood sugar, what to do if levels drop, who to call. A child with seasonal allergies just needs an epinephrine auto-injector on hand. An Individualized Healthcare Plan (IHP) is a written, legally binding document created by the nurse in collaboration with the parent, doctor, and school team. It’s not optional for students with chronic conditions. It’s required under IDEA and Section 504. An IHP includes:- Diagnosis and medical orders
- Medication schedule
- Emergency procedures
- Staff training requirements
- Communication plan with parents
Emergency Meds: Epinephrine and Beyond
Anaphylaxis can kill in minutes. That’s why 87% of U.S. schools now keep stock epinephrine on hand - even for kids who don’t have a diagnosed allergy. But here’s what many don’t know: it must be administered within 5 minutes of symptom onset. Stock epinephrine doesn’t require a specific prescription. It’s a standing order, like fire extinguishers. Nurses train staff to recognize symptoms - hives, swelling, trouble breathing - and act fast. Schools with clear emergency protocols have seen a 40% faster response rate in drills. Other emergency meds? Glucagon for low blood sugar, seizure rescue meds like diazepam nasal spray. These also need clear, practiced procedures. No one should be guessing during a crisis.State Laws Are a Minefield
Here’s the ugly truth: there’s no national standard. Each state has its own Nurse Practice Act. In Texas, some districts treat medication administration as an “administrative task” - meaning anyone can give meds with no nurse oversight. That’s dangerous. A 2022 legal analysis found districts using this model had 14% higher liability risk. In contrast, states like Virginia and California require RN assessment before delegation, mandatory training logs, and nurse approval of all first doses. The NASN’s 2022 guideline is the gold standard - and 37 states still allow delegation under training protocols, while others don’t. School nurses must know their state’s laws inside and out. One wrong move - like letting a teacher give insulin without training - could cost the district millions. Houston ISD was fined $2.3 million in 2022 for medication failures.
Technology Is Changing the Game
The future is digital. As of early 2024, 63% of districts are piloting smartphone-based medication verification systems. These apps let staff scan a barcode on the pill bottle, confirm the student’s ID, log the time, and get a reminder if a dose is missed. Some systems even alert the nurse if a student refuses a dose three times in a week - flagging potential non-adherence or side effects. These tools reduce human error and free up nurse time for care, not paperwork. But tech isn’t magic. It still needs human oversight. A system can’t replace a nurse’s judgment when a child looks pale after taking their med.What Happens When It All Goes Wrong?
Mistakes happen. But how you respond matters. The best districts use a “Just Culture” approach - not blame, but learning. When an error occurs, the nurse leads a non-punitive review:- What went wrong?
- What system failed?
- How do we fix it?
Where to Start: A 7-Step Plan
If your school doesn’t have a solid system, here’s how to build one:- Adopt a district-wide policy using NASN’s sample templates. Allow 8-12 weeks for board approval.
- Train your nurses on delegation, IHPs, and state laws. A 16-hour certification course is standard.
- Screen all students for medication needs. Use categories: Nurse Dependent, Supervised, Self-Administered.
- Create IHPs for every student with a chronic condition. Budget 2-4 hours per student.
- Train unlicensed staff based on medication complexity. Document every session.
- Go digital if possible. EHR systems cut errors and save hours.
- Review monthly - meet with nurses, principals, and parents to discuss near-misses and improvements.
The Bottom Line
Coordinating daily pediatric medications isn’t about paperwork. It’s about trust. Parents trust the school to keep their child safe. Teachers trust the nurse to guide them. And the nurse? They’re the one holding it all together. The system works when:- Every pill is in the right container.
- Every dose is recorded the moment it’s given.
- Every staff member knows what to do - and when to call the nurse.
- Every child with a chronic condition has a plan written down - and followed.
Can a teacher give a student their medication?
Yes - but only if the school nurse has trained and formally delegated the task. The nurse must assess the student’s medical complexity and the staff member’s competency first. For simple oral meds, 4-8 hours of training is typical. For injections or emergency meds, training can be 12-16 hours. The nurse remains legally responsible for the delegation.
Do parents need to bring medications in original bottles?
Yes. Federal law (21 CFR § 1306.22) requires all medications given in school to be in their original, pharmacy-labeled containers. The label must include the student’s name, medication name, dosage, prescriber, and pharmacy info. Ziplock bags or pill organizers are not allowed and put the school at legal risk.
What is an Individualized Healthcare Plan (IHP)?
An IHP is a written plan created by the school nurse, in collaboration with the student’s doctor and parents, for students with chronic health conditions. It outlines medication schedules, emergency procedures, staff training needs, and communication protocols. IHPs are legally required under IDEA and Section 504 for students who need daily medical care at school.
Can a school nurse delegate epinephrine administration to staff?
Yes. Epinephrine auto-injectors are often kept as stock medication in schools, even for students without known allergies. Nurses train staff to recognize anaphylaxis symptoms and administer epinephrine within 5 minutes of onset. This is covered under standing orders and doesn’t require a specific prescription for each student.
How much time should a nurse spend on medication administration daily?
On average, school nurses spend over 2 hours per day on medication documentation and administration alone - and that doesn’t include training staff or updating IHPs. In districts with high student-to-nurse ratios (1:1,102), this workload is unsustainable. Electronic systems can reduce documentation time by 40-45%, freeing nurses to focus on direct care.
What happens if a school doesn’t follow medication protocols?
Non-compliance can lead to legal action, loss of federal funding, or even lawsuits. In 2022, Houston ISD was fined $2.3 million by the Texas Education Agency for medication administration failures. Schools can also be cited for violating Section 504 or IDEA if they don’t provide necessary medical services to students with disabilities.
Is there a shortage of school nurses?
Yes. The national average is 1 nurse for every 1,102 students - far above the recommended 1:750. In some rural areas, it’s 1:3,000. The National Association of School Nurses projects a 15% nursing deficit by 2027. This forces schools to rely more on trained unlicensed staff, increasing the need for strong delegation protocols.
For more support, school nurses can access NASN’s 24/7 consultation line, state school nurse associations, or the CDC’s School Health Guidelines. The goal isn’t perfection - it’s safety. And with the right system, every child can get their medicine - safely, on time, every day.


Tim Tinh
December 9, 2025 AT 07:09Shubham Mathur
December 11, 2025 AT 04:29Ryan Brady
December 12, 2025 AT 15:26Noah Raines
December 13, 2025 AT 02:19Lola Bchoudi
December 14, 2025 AT 13:31Morgan Tait
December 16, 2025 AT 11:55Michael Robinson
December 16, 2025 AT 14:18Andrea Petrov
December 16, 2025 AT 16:34