H2 blocker is a type of medication that reduces stomach acid by blocking histamine H2 receptors on parietal cells. These drugs are a cornerstone in GERD management because they target the source of excess acid without completely shutting it down.
Understanding GERD and Why Acid Matters
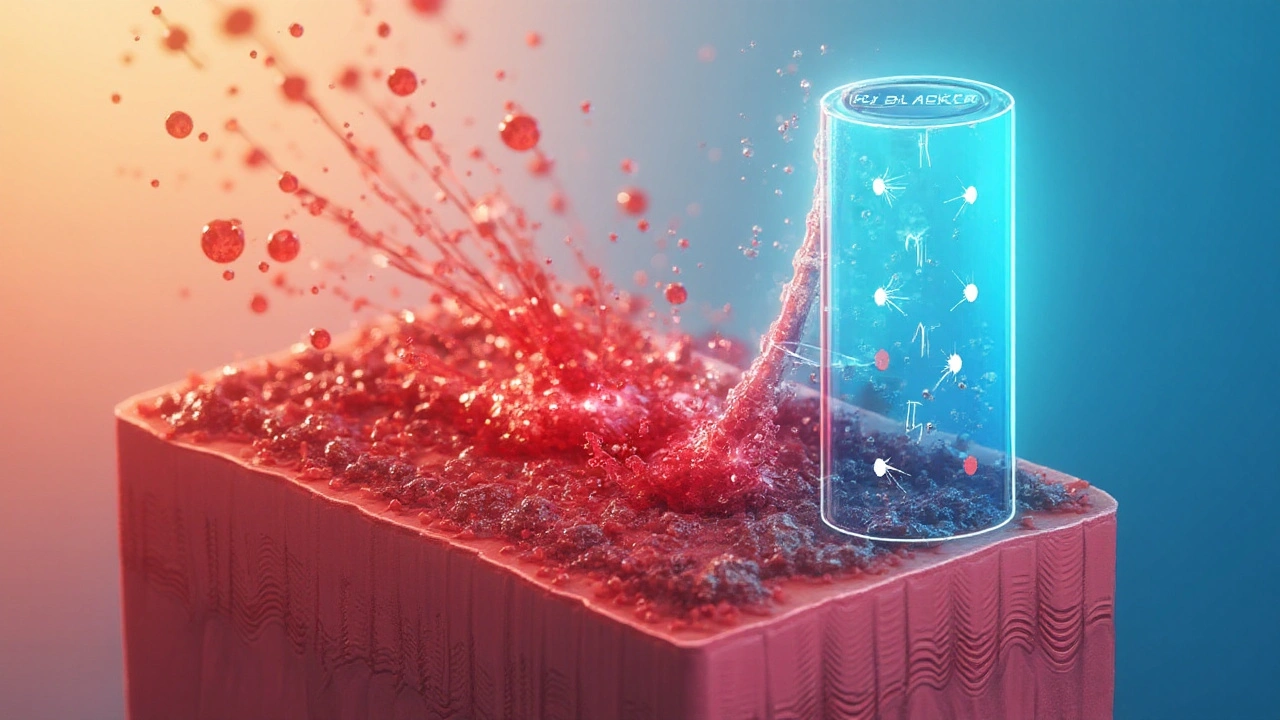
Gastroesophageal reflux disease (GERD) is a chronic condition where stomach contents repeatedly flow back into the esophagus, causing heartburn, regurgitation, and sometimes tissue damage. The underlying problem is often hyper‑secretion of gastric acid, which irritates the esophageal lining. Over time, uncontrolled acid exposure can lead to complications like Barrett's esophagus, a precancerous change in the esophageal lining.
Acid production is driven by three main pathways: gastrin, acetylcholine, and histamine. The histamine pathway acts through the histamine H2 receptor, a protein on the surface of parietal cells that, when stimulated, triggers the release of acid secretion. By blocking this receptor, H2 blockers effectively dial down the amount of acid entering the stomach.
How H2 Blockers Work: The Pharmacology Made Simple
When an H2 blocker binds to the H2 receptor, it prevents histamine from activating the cell. The result is a 30‑60% reduction in basal acid output and a slower rise in acid after meals. This moderation is enough to relieve typical reflux symptoms while preserving enough acidity for normal digestion.
Because the effect is reversible, H2 blockers have a quicker onset (usually 30‑60 minutes) and a shorter duration (8‑12 hours) compared with stronger acid suppressors. This makes them ideal for intermittent or mild‑to‑moderate GERD.
Common H2 Blocker Medications
- Cimetidine - first‑generation H2 blocker, typical dose 200‑400mg twice daily; notable for drug‑interaction potential due to CYP inhibition.
- Famotidine - newer, more selective, 20‑40mg once or twice daily; fewer interactions and a better safety profile.
- Ranitidine - withdrawn in many markets over NDMA impurity concerns, but historically used at 150‑300mg twice daily.
- Nizatidine - less common, 150mg once daily; useful for patients who cannot tolerate other agents.
Each of these drugs shares the same core mechanism but differs in potency, half‑life, and side‑effect spectrum. Choosing the right one depends on patient age, comorbidities, and concurrent medications.
When to Choose an H2 Blocker Over a Proton Pump Inhibitor
Proton pump inhibitors (PPIs) are another major class for GERD. They work downstream by irreversibly inhibiting the H⁺/K⁺‑ATPase pump. While PPIs provide stronger acid suppression, they also carry longer‑term risks such as nutrient malabsorption and infection susceptibility. For patients with intermittent symptoms or those who need a “rescue” medication, H2 blockers are often preferred.
| Attribute | H2 Blocker | Proton Pump Inhibitor |
|---|---|---|
| Mechanism | Blocks histamine H2 receptors | Irreversibly inhibits H⁺/K⁺‑ATPase pump |
| Onset of action | 30‑60 minutes | 1‑2 hours |
| Duration | 8‑12 hours | 24+ hours |
| Typical use | Mild‑to‑moderate, intermittent symptoms | Severe, erosive esophagitis, chronic management |
| Common side effects | Headache, mild dizziness, occasional liver enzyme elevation | Diarrhea, vitamin B12 deficiency, increased infection risk |
The table shows why a doctor might start a patient on an H2 blocker before stepping up to a PPI. It’s a balance of efficacy, safety, and cost.
Dosage, Safety, and Side‑Effect Profile
All H2 blockers are taken orally, usually 30 minutes before meals. The usual adult dosing ranges are:
- Cimetidine: 200mg twice daily (max 800mg/day).
- Famotidine: 20mg once daily (or 40mg twice daily for severe cases).
- Nizatidine: 150mg once daily.
Most side effects are mild: headache, mild nausea, and occasional dizziness. Cimetidine can interfere with drugs metabolized by CYP3A4, so clinicians check for interactions with warfarin, phenytoin, and certain antihistamines.
Renal impairment mandates dose reduction for famotidine and nizatidine. Older adults should start at the lower end of the dose range to avoid confusion with polypharmacy.
Integrating H2 Blockers With Lifestyle Strategies
Medication works best when paired with diet and habit changes. Simple steps that amplify H2 blocker benefits include:
- Avoiding trigger foods (spicy, fatty, citrus, chocolate, caffeine).
- Eating smaller meals and not lying down for at least 2‑3hours after eating.
- Losing excess weight - each 10lb lost can reduce reflux episodes by up to 30%.
- Elevating the head of the bed 6‑8inches to reduce night‑time reflux.
When symptoms return despite these measures, a short‑term “rescue” dose of an H2 blocker (e.g., famotidine 20mg) before bedtime can provide relief without establishing long‑term dependence.
Monitoring Progress and Knowing When to Escalate
Patients should track symptom frequency, severity, and any red‑flag signs such as dysphagia, weight loss, or vomiting. If symptoms persist after 4‑6 weeks of optimal H2 blocker therapy, an endoscopic evaluation is warranted to rule out erosive esophagitis or Barrett’s esophagus.
In such cases, a physician may transition to a PPI or consider combination therapy (H2 blocker at bedtime plus PPI in the morning) for refractory disease.
Key Take‑aways
- H2 blockers reduce acid by blocking histamine H2 receptors, offering a moderate and fast‑acting solution.
- They are ideal for mild‑to‑moderate GERD, intermittent symptoms, or as rescue medication.
- Common agents-cimetidine, famotidine, nizatidine-differ in potency and interaction risk.
- Compared with PPIs, H2 blockers have a quicker onset, shorter duration, and fewer long‑term safety concerns.
- Pairing medication with lifestyle adjustments maximizes relief and may prevent the need for stronger drugs.

Frequently Asked Questions
Can I take an H2 blocker and a PPI at the same time?
In some cases, doctors prescribe a low‑dose H2 blocker at night to prevent nighttime acid spikes while a PPI handles daytime production. This combo should only be used under medical supervision because overlapping effects can increase side‑effects.
How long is it safe to use H2 blockers?
Short‑term use (up to 12 weeks) is generally safe for most adults. Long‑term therapy is possible but requires periodic liver function tests for cimetidine and kidney monitoring for famotidine or nizatidine.
Do H2 blockers work for heartburn caused by pregnancy?
Yes, famotidine is often considered safe in pregnancy and can alleviate reflux without affecting the fetus. However, any medication during pregnancy should be approved by a healthcare provider.
Why was ranitidine removed from the market?
Regulators found that some ranitidine products contained NDMA, a probable carcinogen, at levels above acceptable limits. The risk led to a worldwide withdrawal in 2020‑2021.
Can H2 blockers cause vitamin deficiencies?
Unlike PPIs, H2 blockers have a minimal impact on nutrient absorption. Long‑term use rarely leads to deficiencies, but routine blood tests are still advisable for chronic users.
What should I do if I miss a dose?
Take the missed dose as soon as you remember unless it’s close to the next scheduled dose. In that case, skip the missed one - don’t double up, as higher doses increase side‑effect risk.
Are there natural alternatives to H2 blockers?
Lifestyle changes (weight loss, diet, sleep‑elevation) are the first line. Some herbal teas (ginger, chamomile) may soothe symptoms, but they don’t reduce acid production like H2 blockers do.


Mansi Mehra
September 25, 2025 AT 23:33The article accurately distinguishes H2 blockers from proton pump inhibitors. The explanation of receptor blockade is concise. No typographical errors were observed.
Krista Evans
October 4, 2025 AT 13:57Hey there, great job breaking down the science behind H2 blockers-so clear and helpful! It really shows how a simple medication can make a huge difference in daily comfort. I love how you paired the drug info with lifestyle tips; that combo is a game‑changer for anyone dealing with reflux. Keep encouraging people to stay active and watch their meals, because those little habit tweaks can cut symptoms dramatically. And the reminder to track symptoms is spot on-self‑monitoring is the best way to know when it’s time to see a doc. Your upbeat tone makes the whole thing feel doable, not intimidating. Also, the table comparing H2 blockers and PPIs is a fantastic visual aid; I’ll definitely share that with friends. Remember, patience is key-sometimes it takes a few weeks to see the full benefit. If anyone feels stuck, a short‑term “rescue” dose before bedtime, like you suggested, can be a lifesaver. Thanks for making complex pharmacology feel like a friendly chat over coffee. Keep up the awesome work, and keep spreading that positive, supportive vibe!
Mike Gilmer2
October 13, 2025 AT 04:21Whoa, this read was like a roller‑coaster through the acid battlefield! The way you described histamine’s role had me on the edge of my seat. I could almost hear the parietal cells screaming, "Not today!" The drama of H2 blockers versus PPIs is epic-like heroes vs. villains in a medical saga. Your table reads like a showdown in a comic book, and I’m here for the plot twists. Even the side‑effects list has that suspenseful feel of a cliffhanger. Kudos for turning a textbook topic into a blockbuster!
Alexia Rozendo
October 21, 2025 AT 18:45Sure, because we all needed a dramatized acid fight to understand basic pharmacology. Nice effort, though.
Kimberly Newell
October 30, 2025 AT 08:09Hey folks, just wanted to add a quick note – the info here is super useful, especially for those of us juggling a lot. I think it might be helpful to remember that staying hydrated can also calm the stomach, even if it’s not a direct meds effect. Definately keep an eye on med interactions, especially if you’re takin any other meds. Also, try to avoid eating right before bed – it really makes a difference. Thanks for sharing all this great advice, it’s really recommneded for anyone dealing with reflux.
Jacob Hamblin
November 7, 2025 AT 22:33Great summary! Just a tiny suggestion: you might want to add a comma after "short‑term" in the sentence about rescue dosing – it reads a bit smoother. Other than that, the explanation is spot on and very friendly. Thanks for making the complex stuff feel approachable.
Andrea Mathias
November 16, 2025 AT 12:57Holy hell, those PPIs are the corporate poison they don’t want you to know about!
TRICIA TUCKER
November 25, 2025 AT 03:21Oh wow, love the energy! Just a heads‑up, "cimetidine" should be spelled with an "i" after the "m" – small detail, but important for clarity. Also, your table looks awesome; maybe add a footnote for the NDMA issue with ranitidine, just to keep readers fully informed. Keep the vibe upbeat, it really helps people feel less scared about meds.
Dave Tu
December 3, 2025 AT 17:45While the article is thorough, it glosses over the significant long‑term risks associated with chronic H2 blocker use, such as potential renal concerns. Moreover, the claim that H2 blockers have minimal impact on nutrient absorption lacks robust citation. One must also consider the economic incentives driving pharmaceutical promotion of these agents. A more critical perspective would benefit readers, especially those questioning the safety profile.
Johnna Sutton
December 12, 2025 AT 08:09It is quite astonishing how mainstream med journals conveniently omit the hidden agenda of big pharma in pushing H2 blockers. Some might say there is a coordinated effort to keep the public unaware of alternative natural remedies, which are subtly suppressed. The official narrative is highly formal, yet the underlying truth is far from transparent. One should always question the source and look for the suppressed data that reveals the true risk.
Vinay Keragodi
December 20, 2025 AT 22:33Reading through this, I’m struck by how well the pharmacology is explained without drowning the reader in jargon. It’s nice to see the balance between medication and lifestyle adjustments – that holistic view is often missing. I wonder, though, if there’s any data on how diet alone compares to H2 blocker efficacy in mild cases. Also, the mention of renal dose adjustments is a good reminder for older adults. Overall, an informative piece that feels both scientific and accessible.