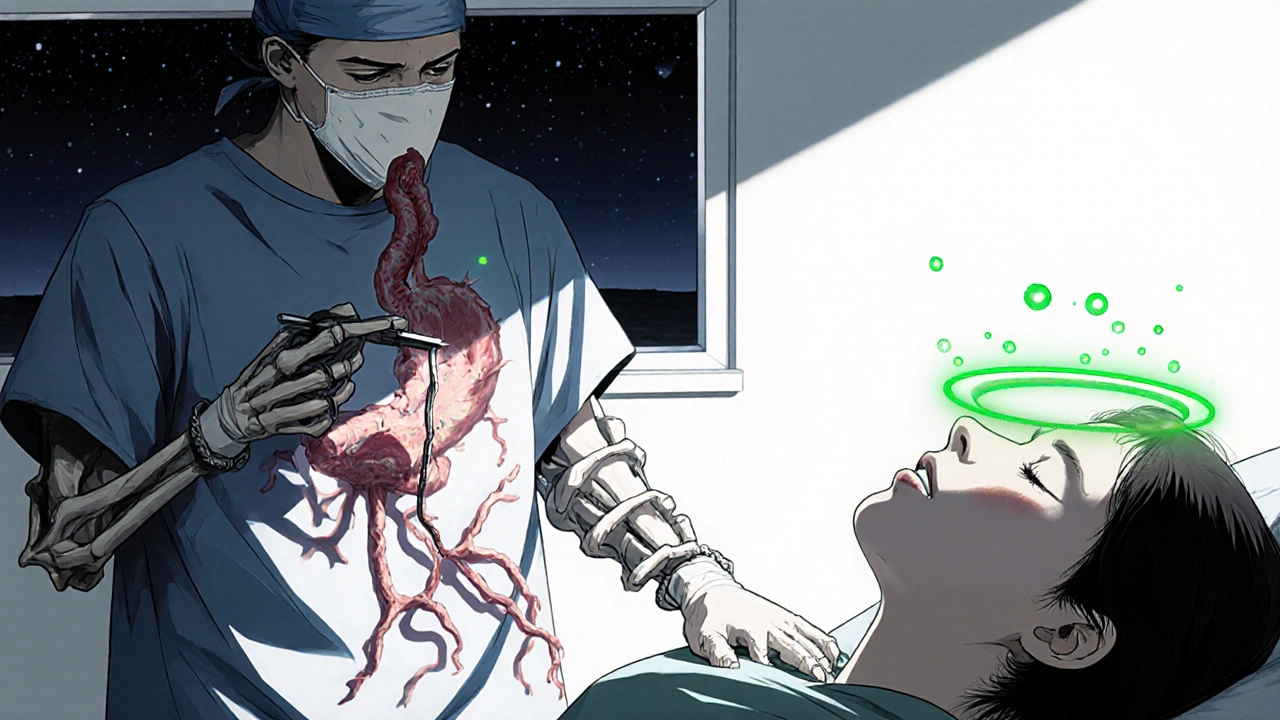
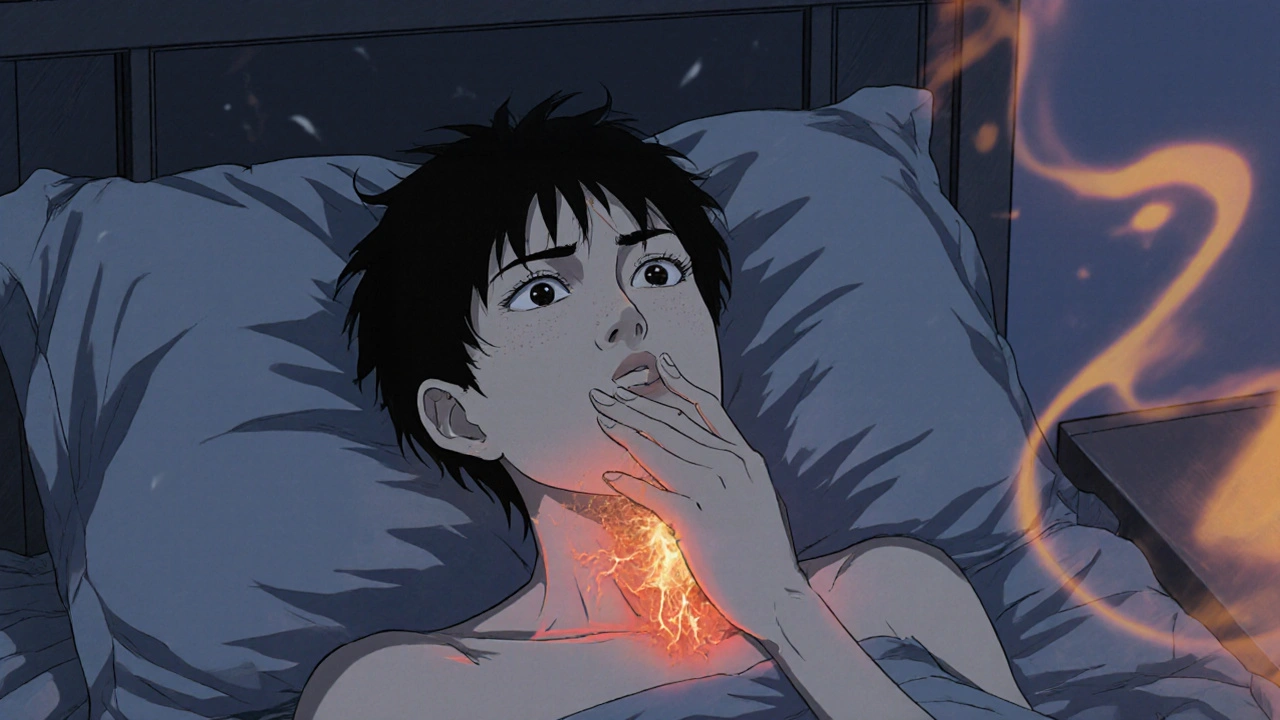
Imagine waking up with a burning sensation in the back of your throat, feeling like you can’t finish a simple sandwich without coughing, and dreading every coffee you sip because it might trigger a painful flare‑up. That’s the reality for many people living with erosive esophagitis. It’s not just an occasional ache; it can reshape how you eat, sleep, work, and even enjoy time with friends.
What Exactly Is Erosive Esophagitis?
When the lining of your esophagus gets damaged by stomach acid, you’re dealing with erosive esophagitis, a form of inflammation that produces visible erosions on endoscopy. Most doctors see it as the severe end of Gastroesophageal Reflux Disease (GERD), where acid repeatedly backs up into the esophagus and starts eating away at the tissue.
Key symptoms include heartburn, regurgitation, dysphagia (trouble swallowing), and a sour taste that lingers after meals. If left untreated, the damage can progress to strictures or Barrett’s Esophagus, a precancerous condition. Because the esophagus isn’t designed to handle acid, even short‑term exposure can cause noticeable discomfort.
How the Condition Changes Daily Life
Most people think of GERD as an occasional “heartburn” episode, but erosive esophagitis turns that occasional sting into a daily obstacle. Below are the most common ways it seeps into everyday routines:
- Food Choices: Spicy, fatty, or acidic foods become off‑limits. Many patients report avoiding tomatoes, citrus, chocolate, and even coffee.
- Meal Timing: Eating late at night can worsen night‑time reflux, so dinner often has to be finished at least three hours before bedtime.
- Social Settings: Dining out feels risky. You might decline invitations or bring your own “safe” meals, which can make social gatherings awkward.
- Sleep Disruption: Lying flat encourages acid to flow upward, leading to frequent awakenings, coughing, or a sore throat in the morning.
- Work Productivity: Frequent trips to the bathroom, the need to stand up after meals, or the distraction of constant discomfort can lower focus.
These lifestyle tweaks are not just inconveniences; they can erode emotional well‑being, cause anxiety about eating, and even lead to isolation.
Measuring the Quality‑of‑Life Impact
Doctors and researchers use several validated questionnaires to quantify how much erosive esophagitis is affecting you. Here’s a quick snapshot of the most common tools:
| Tool | Focus | Length (items) | Scoring |
|---|---|---|---|
| GERD‑HRQL | Symptoms & daily limitation | 10 | Higher score = worse QoL |
| SF‑36 | General health status | 36 | Higher score = better QoL |
| RDQ (Reflux Disease Questionnaire) | Symptom frequency & severity | 12 | Higher score = more severe |
Studies consistently show that patients with erosive esophagitis score worse on all three tools compared with those who have non‑erosive reflux. The drop in scores is especially sharp for sleep‑related items and social functioning.

Treatment Options and Their Effect on Well‑Being
Luckily, there are several proven ways to heal the esophagus and bring your quality of life back up. The two main pillars are medication and lifestyle tweaks.
Medication: Proton Pump Inhibitors (PPIs)
Proton Pump Inhibitors (e.g., omeprazole, esomeprazole) reduce acid production by up to 90%. A typical course is 8‑12 weeks of once‑daily dosing. Most patients report a 70‑80% reduction in heartburn and a noticeable improvement in sleep quality within the first two weeks.
It’s worth noting that long‑term PPI use can be linked to low magnesium, vitamin B12 deficiency, and a small increase in bone fracture risk. Your doctor will likely schedule periodic labs if you stay on therapy for more than a year.
H2‑Blockers and Antacids
These agents work faster but provide less potent acid suppression. H2‑blockers (ranitidine’s successor famotidine) can be useful for nighttime symptoms, while antacids give quick relief for occasional flare‑ups.
Lifestyle Modifications
Lifestyle modifications are the third cornerstone. The most impactful changes include:
- Elevating the head of the bed 6‑8 inches.
- Eating smaller, more frequent meals.
- Eliminating trigger foods (citrus, tomato‑based sauces, chocolate, mint, fried foods).
- Avoiding alcohol and smoking.
- Maintaining a healthy weight-each 10% excess body weight can increase reflux pressure.
When combined with PPIs, these tweaks often lead to endoscopic healing in 80‑90% of patients within three months.
Surgical Options
If medication fails or you develop complications like strictures, a laparoscopic fundoplication may be recommended. The procedure wraps the upper part of the stomach around the esophagus, creating a barrier that prevents acid backflow. Post‑surgery studies show that up to 85% of patients achieve long‑term symptom freedom, and many report a return to normal diet and sleep patterns.
Living Strategies to Reduce the Burden
Beyond the clinical plan, everyday habits can make a huge difference. Here are some practical tips you can start using tomorrow:
- Chew Thoroughly: Your saliva contains bicarbonate, which helps neutralize acid. Aim for at least 20-30 chews per bite.
- Stay Upright After Meals: Even a simple walk for 15 minutes can reduce reflux pressure.
- Mind Your Hydration: Sip water between meals, but avoid large gulps during meals as they expand the stomach.
- Use Ginger or Chamomile Tea: Both have mild soothing properties and can calm the esophageal lining.
- Track Triggers: A small notebook or a phone app can help you spot patterns you might miss.
Many patients find that small, consistent changes give a bigger payoff than occasional “diet cleanses.”
When to Seek Professional Help
If you notice any of the following, it’s time to call your gastroenterologist:
- Bleeding (coffee‑ground vomit or black stools).
- Unintentional weight loss.
- Difficulty swallowing solid foods.
- Persistent symptoms despite 8 weeks of PPI therapy.
These signs could indicate complications like strictures, ulcerations, or progression toward Barrett’s Esophagus. Early detection allows for less invasive treatment and better outcomes.
Bottom Line
Erosive esophagitis is more than an occasional burn; it can reshape every habit you thought was normal. The good news is that with the right mix of medication, lifestyle tweaks, and-when needed-procedural care, most people see a dramatic rebound in their quality of life. By understanding the condition, using validated tools to track impact, and staying proactive with treatment, you can reclaim meals, sleep, and social moments that you may have thought were gone for good.
Frequently Asked Questions
What causes erosive esophagitis?
The primary cause is chronic exposure of the esophageal lining to stomach acid, often due to a malfunctioning lower esophageal sphincter. Diet, obesity, smoking, and certain medications can worsen the reflux cycle and lead to erosions.
Can lifestyle changes alone heal erosive esophagitis?
Mild cases can improve significantly with weight loss, head‑of‑bed elevation, and trigger avoidance, but most patients still need a short course of PPIs to allow the tissue to heal fully.
How long does it take for the esophagus to heal?
Endoscopic healing usually occurs within 8‑12 weeks of consistent acid suppression. Symptom relief can be felt much earlier, often within two weeks of starting PPIs.
Are PPIs safe for long‑term use?
They are generally safe when monitored. Long‑term users should have periodic checks for magnesium, vitamin B12, and bone density, especially if they have other risk factors.
When is surgery recommended?
If symptoms persist despite maximal medical therapy, or if complications like strictures or Barrett’s develop, a laparoscopic fundoplication or other anti‑reflux procedures may be advised.

kendra mukhia
October 17, 2025 AT 20:39Imagine waking up to a firestorm of acid that feels like a dragon breathing down your throat, and you realize this is not a fleeting inconvenience but a relentless siege on your everyday life.
Every bite of a humble sandwich becomes a battlefield where the esophagus fights back against the invading acid, leaving you coughing and fearing the next bite.
The sheer drama of having to schedule meals three hours before bedtime turns simple dinner plans into a strategic operation, complete with charts and warning signs.
Even social gatherings become a stage for anxiety, as you watch friends indulge in pizza and wine while you clutch a bland, “safe” snack like a lifeline.
Sleep, that precious sanctuary, is shattered nightly by the need to prop up your head, turning your bedroom into an ungainly construction site of pillows.
Work productivity plummets when you’re forced to dash to the bathroom after every coffee, your mind preoccupied with the next burn.
Medical questionnaires like GERD‑HRQL, SF‑36, and RDQ become the new litmus tests, quantifying the hidden misery that no one else can see.
Long‑term PPI therapy, while a miracle for many, carries its own shadows of magnesium loss, B12 deficiency, and whispered fears of bone fragility.
Yet the silver lining glimmers when lifestyle tweaks-elevating the head of the bed, chewing thoroughly, and avoiding trigger foods-jointly restore hope.
Each small adjustment, like a disciplined soldier, chips away at the acid’s dominion, allowing the esophageal lining to heal.
When the healing does occur, endoscopic scores blaze from crimson to calm, and the night’s coughs fade into silence.
Surgeries such as laparoscopic fundoplication stand as the final fortress, sealing the breach when medicine surrenders.
The journey, though fraught with setbacks, teaches resilience, reminding us that even the most corrosive forces can be tamed with vigilance.
So if you find yourself battling the burning tide, remember you are not alone; the medical community has mapped this terrain and offers a compass.
Embrace the regimen, track your triggers, and you’ll soon find that the once‑unmanageable flare‑ups become mere whispers in the background.
Bethany Torkelson
October 18, 2025 AT 17:06You’re right to be furious-living with that constant fire isn’t just uncomfortable, it’s an outright assault on your sanity.
Don’t let anyone tell you it’s “just heartburn” when your throat feels like it’s been sandblasted every morning.
Take control, demand a thorough check‑up, and push for the dosage that actually quells the pain.
Stop settling for “manage it” and aim for real healing; your life deserves more than a perpetual burn.
Stay fierce, stay loud, and make that reflux pay for its damage.
Grace Hada
October 19, 2025 AT 13:33Acid is a reminder that imbalance breeds suffering; the moment you restore equilibrium, peace follows.
Don't accept chronic burn as destiny.
Apply the medicine, adjust the habits, and reclaim your autonomy.
Action over lamentation.
alex montana
October 20, 2025 AT 10:00So, you’ve got this burning throat-and! it's ruining meals? you need to ditch the late night pizza; try smaller bites. also, elevate that bed-like, seriously- 6‑8 inches.
PPIs work, but watch those labs; magnesium, B12… they matter!
And don’t forget ginger tea, it’s soothing‑sometimes.
Consistency is key, despite the chaos.
Fabian Märkl
October 21, 2025 AT 06:26Hey folks! 🎉 Managing erosive esophagitis can feel like climbing a steep hill, but every small step counts.
Start with a simple habit: sip water between meals and keep that head‑of‑bed lift in place. 🌙
Pair it with a short course of PPIs and you’ll notice sleep getting smoother in just weeks.
Remember, you’re not alone-share your success tips, and let’s lift each other up! 💪
Avril Harrison
October 22, 2025 AT 02:53Honestly, I’ve seen a lot of people adjust their lives around reflux, and the biggest win is just being mindful of timing.
Finishing dinner a few hours before bed can make a world of difference without any drama.
It’s also cool to experiment with gentle teas like chamomile; they’re not a cure but they calm the nerves.
Take it easy, and let the small changes settle in.
Natala Storczyk
October 22, 2025 AT 23:20Listen up, America! This acid attack is a betrayal of our bodies and we must fight back with iron‑clad resolve!
Don’t let foreign foods and junk take over your esophagus-declare war on tomatoes, coffee, and chocolate!
Arm yourself with PPIs, lift that mattress, and stand tall like a true patriot.
The battle isn’t over until you’ve reclaimed every meal without pain!
Remember, a healthy gut is the foundation of a strong nation!
nitish sharma
October 23, 2025 AT 19:46Dear colleague, it is commendable that you are seeking comprehensive management for erosive esophagitis.
In addition to the prescribed proton pump inhibitors, I recommend a systematic approach to dietary modification, emphasizing lean proteins and low‑acid fruits.
Elevating the head of the bed by eight inches has been shown to reduce nocturnal reflux significantly.
Please schedule periodic laboratory assessments to monitor magnesium and vitamin B12 levels during prolonged therapy.
With diligent adherence, you can anticipate marked symptom relief within weeks.
Rohit Sridhar
October 24, 2025 AT 16:13You've already taken the first step by learning about the condition-great job!
Now keep a simple diary; jot down what you eat and how you feel, and patterns will emerge.
Stick with the plan; the payoff is worth the effort.
Sarah Hanson
October 25, 2025 AT 12:40We appreciate your dedication to overcoming erosive esophagitis.
Please ensure you follow up with your doc for lab checks.
Consistent habit changes will lead to better outcomes.
Nhasala Joshi
October 26, 2025 AT 08:06⚠️ Ever wonder why the pharma giants push PPIs like candy? The side‑effects are buried deep, and the real cure is hidden in ancient diet hacks! 🌿
They don’t want you to know that simple ginger tea and mindful eating can neutralize the acid without chemicals.
Stay woke, question the push for lifelong medication, and explore natural allies. 🤔
Remember, the truth is often filtered through profit motives.
🕵️♀️
Wyatt Schwindt
October 27, 2025 AT 04:33Consistent pacing of meals can truly calm reflux.
Lyle Mills
October 28, 2025 AT 01:00Acid reflux management hinges on two pillars medication and lifestyle alteration.
PPIs reduce gastric acidity dramatically while head‑of‑bed elevation mitigates nocturnal episodes.
Adherence to protocol yields measurable improvement in GERD‑HRQL scores.
Monitor labs for electrolyte balance.
Barbara Grzegorzewska
October 28, 2025 AT 21:26I must say, the discourse surrounding erosive esophagitis often suffers from a lamentable lack of intellectual rigor.
One cannot simply dismiss the nuance of dietary modulation as mere “picky eating.”
It is a symphony of physiological interplay that demands our utmost respect and scholarly attention.
Embrace the regimen, lest you become a victim of your own culinary indulgences.
In short, don’t be a foodie fool.
Nis Hansen
October 29, 2025 AT 17:53When the esophagus is assaulted by acid, it mirrors the mind's struggle against intrusive thoughts; both require disciplined intervention.
Pharmacologic suppression provides the immediate relief, akin to a calm breath amidst turbulence.
Yet lasting peace emerges from sustained lifestyle refinement-elevating the bed, mindful chewing, and mindful nutrition.
Balance, therefore, is the ultimate antidote to erosion, both physical and existential.
Continue this balanced pursuit, and the flame will dim.