Allergy Trigger Identifier
Answer the following questions to identify possible allergy triggers and understand your immune response:
Your Allergy Profile:
When allergies flare up, many people feel miserable, but the real drama is happening inside the body’s defense network. Below we unpack exactly how those irritating reactions mess with the immune system, what that means for everyday health, and what you can do to keep the balance in check.
Quick Summary
- Allergies are hypersensitive immune reactions triggered by harmless substances called allergens.
- The key player is IgE, an antibody that flags allergens and activates mast cells.
- When mast cells release histamine and other mediators, you get classic symptoms like itching, swelling, and airway constriction.
- Repeated exposure can shift the immune response, leading to chronic inflammation or even autoimmune‑like effects.
- Managing exposure, supporting gut health, and using targeted antihistamines can restore equilibrium.
What Exactly Are Allergies?
Allergies are exaggerated immune responses to substances that are otherwise harmless. Common culprits-known as Allergens-include pollen, pet dander, certain foods, and insect venom. When an allergen enters the body, a sensitized immune system mistakenly treats it as a threat.
Allergy types can be grouped into three broad categories:
- Respiratory (e.g., hay fever, asthma triggers)
- Dermatologic (e.g., eczema, contact dermatitis)
- Food‑related (e.g., peanuts, shellfish)
Each type follows a similar pathway, but the tissues affected and the severity of symptoms vary.
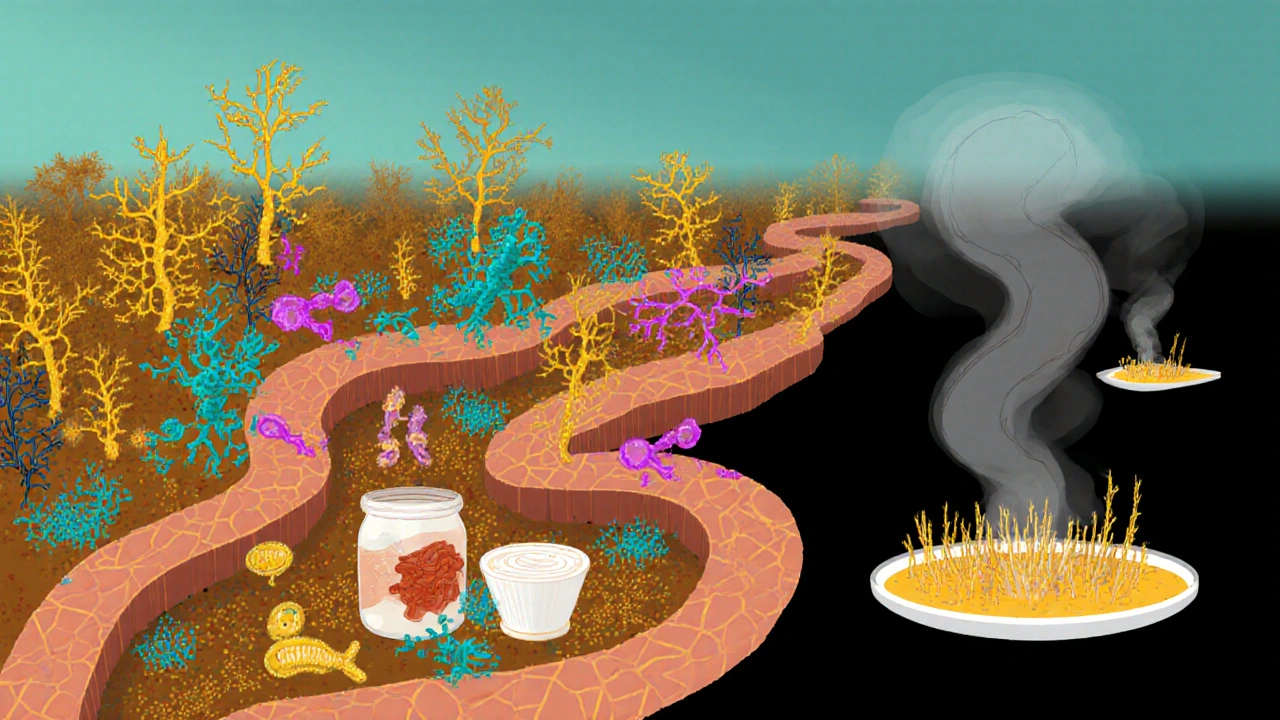
How the Immune System Normally Works
The immune system is a complex network of cells, proteins, and signaling molecules. Its job is to identify and eliminate pathogens while leaving the body’s own cells untouched. Key components include:
- White blood cells (leukocytes) like Mast Cells and basophils.
- Antibodies such as IgE, which specialize in recognizing allergens.
- Chemical messengers-Cytokines and Histamine-that coordinate inflammation and healing.
In a healthy response, antibodies like IgG neutralize viruses and bacteria, while IgE levels stay low. The system maintains a delicate balance between activation and tolerance.
The Allergy‑Immune Interaction
When an allergen first meets a sensitized individual, the following cascade unfolds:
- Sensitization: Dendritic cells pick up the allergen and present it to T‑helper cells, which then stimulate B‑cells to produce IgE antibodies specific to that allergen.
- Binding: The newly minted IgE circulates and latches onto high‑affinity receptors on Mast Cells and basophils, essentially “arming” them.
- Re‑exposure: When the same allergen re‑enters the body, it cross‑links the IgE on mast cells, triggering an immediate degranulation.
- Release of Mediators: Histamine, leukotrienes, prostaglandins, and various Cytokines pour into surrounding tissue.
- Symptoms Appear: Histamine widens blood vessels, attracts more immune cells, and irritates nerves-causing itching, swelling, mucus, and airway tightening.
This rapid response is what we recognize as a sneeze, rash, or wheeze. It’s a short‑term protective mechanism, but the repeated activation can wear down the system.
Short‑Term vs Long‑Term Effects on the Immune System
Short‑Term: Acute releases of histamine and cytokines generate inflammation that clears the allergen quickly. However, this also drains cellular reserves and temporarily suppresses other immune functions, making you a bit more vulnerable to infections right after a severe flare.
Long‑Term: Chronic exposure-think daily pollen or constant pet dander-keeps mast cells in a semi‑activated state. Over time, this leads to:
- Elevated baseline Cytokine levels, contributing to systemic inflammation.
- Altered gut microbiota, which influences immune tolerance and can predispose to new sensitivities.
- Potential overlap with autoimmune processes, where the immune system starts attacking self‑tissues because regulatory pathways are exhausted.
Research from 2023‑2024 shows that people with severe allergic rhinitis have a 15% higher risk of developing autoimmune thyroiditis, underscoring how chronic allergy stress can spill over.
Managing the Impact - Practical Strategies
Breaking the cycle requires both exposure control and immune support:
- Identify Triggers: Keep a symptom diary. Note foods, locations, and weather conditions that precede flare‑ups.
- Environmental Controls: Use HEPA filters, wash bedding in hot water weekly, and keep windows closed during high pollen counts.
- Nutrition for Tolerance: Probiotic‑rich foods (yogurt, kimchi) and omega‑3 fatty acids help modulate inflammatory cytokine production.
- Targeted Medications: Antihistamines block histamine receptors, reducing immediate symptoms. For severe cases, allergen‑specific immunotherapy (desensitization shots) retrains IgE production.
- Lifestyle Adjustments: Regular moderate exercise improves overall immune regulation, while adequate sleep curbs cytokine spikes.
When choosing an antihistamine, consider whether you need a first‑generation (sedating) or second‑generation (non‑sedating) agent. Second‑generation drugs like cetirizine have a faster onset and fewer daytime drowsiness issues.
Emerging Research - What’s on the Horizon?
Scientists are exploring several promising avenues:
- Biologic Therapies: Monoclonal antibodies such as omalizumab bind free IgE, dramatically lowering mast‑cell activation for severe asthma and chronic urticaria.
- Microbiome Modulation: Fecal transplant studies suggest that restoring a diverse gut flora can reset immune tolerance, reducing allergy prevalence.
- Peptide Vaccines: Small allergen fragments are being tested to safely teach the immune system to ignore the full protein without triggering a full‑blown response.
These advances aim to move beyond symptom control and actually re‑educate the immune system.
Allergy Types, Common Triggers & Typical Immune Mechanism
| Allergy Type | Typical Triggers | Immune Pathway |
|---|---|---|
| Respiratory (Hay Fever) | Pollen, mold spores | IgE‑mediated mast‑cell degranulation → histamine release → nasal congestion |
| Food Allergy | Peanuts, shellfish, milk | IgE binds to gut mast cells → histamine + leukotrienes → hives, anaphylaxis |
| Contact Dermatitis | Nickel, latex, fragrances | IgE‑independent T‑cell mediated inflammation → cytokine surge |
| Drug Allergy | Penicillins, NSAIDs | IgE or direct mast‑cell activation → rash, fever |
Bottom Line - Keeping Your Immune System Balanced
Allergies are more than just itchy eyes; they’re a persistent stress test for the immune system. By recognizing triggers, supporting gut health, and using precise medication, you can reduce both the short‑term misery and the long‑term inflammatory burden.

Frequently Asked Questions
Why do some people develop allergies while others don’t?
Genetics set the baseline, but environmental factors-like early‑life exposure to microbes, diet, and pollution-shape how the immune system learns to tolerate harmless substances. A family history of atopy (asthma, eczema, hay fever) raises the odds, but lifestyle can tip the balance either way.
Can allergies lead to autoimmune diseases?
Chronic allergic inflammation raises systemic cytokine levels, which can stress regulatory T‑cells that keep autoimmunity in check. Studies have linked severe allergic rhinitis and asthma with higher rates of conditions like type‑1 diabetes and autoimmune thyroiditis.
Are antihistamines safe for long‑term use?
Second‑generation antihistamines are generally well‑tolerated for years, but they can cause mild dry mouth or fatigue in some people. It's wise to rotate or take breaks under a doctor’s guidance, especially if you notice persistent side effects.
What role does the gut microbiome play in allergies?
A diverse gut flora helps train immune cells to distinguish friend from foe. Low diversity-common after antibiotics or a high‑sugar diet-correlates with higher IgE levels and more severe allergic responses. Probiotic supplements and fermented foods can restore balance.
Is allergy immunotherapy effective for adults?
Yes. A series of gradually increasing allergen exposures-either via injection or sublingual tablets-can reduce IgE production and increase IgG4, a blocking antibody. Most adults see a 30‑60% reduction in symptoms after 3‑5 years of treatment.


Stephen Gachie
September 30, 2025 AT 21:01Allergies expose a paradox: the immune system, designed to protect, becomes the aggressor when faced with benign molecules. When IgE binds to mast cells, the body treats pollen like an invader, releasing histamine in a cascade that feels both logical and absurd. This duality invites reflection on how our biology negotiates danger and safety, a dialogue as old as evolution itself.
Sara Spitzer
October 2, 2025 AT 00:47The article oversimplifies the role of the microbiome, ignoring the nuanced studies that show strain‑specific effects on IgE modulation. Moreover, the suggested “HEPA filter” remedy is presented without acknowledging the variable efficacy across indoor environments. A more rigorous citation of recent meta‑analyses would strengthen the claims.
Anshul Gandhi
October 3, 2025 AT 04:34What the piece fails to mention is the hidden agenda of pharmaceutical conglomerates that profit from chronic antihistamine sales. By framing allergies as an inevitable nuisance, they push a narrative that keeps us dependent on their products, while silencing research into true immune tolerance strategies. It’s a classic case of manufactured demand.
Emily Wang
October 4, 2025 AT 08:21Don’t let a sneeze stall your momentum-think of each symptom as a signal to optimize your environment and your body. Small steps like swapping pillowcases weekly and adding a probiotic shake can tip the balance toward resilience. Keep pushing, the relief is worth the effort.
Hayden Kuhtze
October 5, 2025 AT 12:07Oh sure, just toss a HEPA filter in the corner and expect miracles-because allergens are that obedient.
Craig Hoffman
October 6, 2025 AT 15:54Allergy management starts with accurate identification of triggers
Keeping a detailed symptom diary helps correlate exposure with reactions
Environmental controls such as air purifiers reduce airborne pollen load
Regular washing of bedding in hot water eliminates dust mites
Dietary adjustments, especially reducing high‑histamine foods, can lessen flare‑ups
Probiotics support gut flora which in turn influences IgE production
Omega‑3 fatty acids from fish oil have anti‑inflammatory properties
First‑generation antihistamines may cause drowsiness, consider second‑generation alternatives
Immunotherapy, whether injections or sublingual tablets, retrains the immune system over months
Patients often notice a 30‑60% reduction in symptoms after consistent therapy
Stress management through meditation or moderate exercise improves overall immune regulation
Adequate sleep restores cytokine balance and reduces baseline inflammation
Avoid smoking and limit alcohol as they can exacerbate histamine release
Consult an allergist to tailor a personalized plan rather than self‑medicating
Stay updated with emerging biologic treatments like anti‑IgE monoclonal antibodies
Overall, a holistic approach that combines lifestyle, environmental, and medical strategies yields the best outcomes
Terry Duke
October 7, 2025 AT 19:41Wow, you really hit the nail on the head, Sara! The lack of depth in the microbiome section is glaring, and the HEPA suggestion? It feels like a quick fix, not a solution. I love how you called for proper citations-science deserves that rigor! Let’s hope future updates address these gaps, because readers deserve better, don’t they?
Chester Bennett
October 8, 2025 AT 23:27Great summary, Craig. Your step‑by‑step checklist is practical and easy to follow. I especially appreciate the emphasis on sleep and stress management, often overlooked in allergy discussions. Keep sharing such actionable advice!
Emma French
October 10, 2025 AT 03:14Allergy shots are a game‑changer, no doubt.
Ken Elelegwu
October 11, 2025 AT 07:01When we examine allergies through the lens of epistemology, we uncover a deeper truth about the body’s capacity to label the benign as hostile. This mislabeling is not merely a biochemical error but a narrative our immune system has been taught to repeat. Restoring tolerance, therefore, is akin to rewriting a story we have long accepted. The emerging microbiome research hints at a collective memory stored in our gut flora, waiting to be re‑educated. By nurturing diversity in that ecosystem, we may coax the immune system into a more compassionate stance. It's a subtle rebellion against the entrenched paradigm of perpetual vigilance. Embrace this shift, and the symptoms may recede as the story changes.
Gene Nilsson
October 12, 2025 AT 10:47It is unequivocally the moral imperative of the medical community to ensure that patients are not subjected to the pernicious effects of chronic antihistamine usage without rigorous oversight. The proliferation of over‑the‑counter remedies, while ostensibly benevolent, oftentimes possibily obfuscates the underlying pathology and fosters a complacent attitude towards true curative interventions. Therefore, I implore physicians and regulatory bodies alike to reevaluate the prevailing standards, lest we continue to perpetuate a cycle of temporary solace at the expense of long‑term health.
Vintage Ireland
October 13, 2025 AT 14:34Hey, I totally get how exhausting allergy flare‑ups can be. It’s easy to feel like your body’s working against you, but remember you’re not alone in this. Small wins, like a fresh air filter or a calming tea, can add up over time. Keep sharing what helps you, and we’ll all learn together.