H1 vs H2 Blocker Symptom Checker
Select Your Symptoms
Choose the symptoms you're experiencing to determine which blocker type is appropriate
Recommendation
Important Safety Note
H1 and H2 blockers are NOT interchangeable. Never mix them without medical supervision. Taking H1 blockers for heartburn or H2 blockers for allergies will not resolve your symptoms.
Most people know antihistamines for stopping sneezing and itchy eyes, but not everyone realizes there are two major types with very different jobs. H1 blockers handle allergies. H2 blockers handle stomach acid. They both block histamine, but they target different parts of your body-and that changes everything about how they work, what side effects you get, and when you should take them.
What H1 Blockers Actually Do
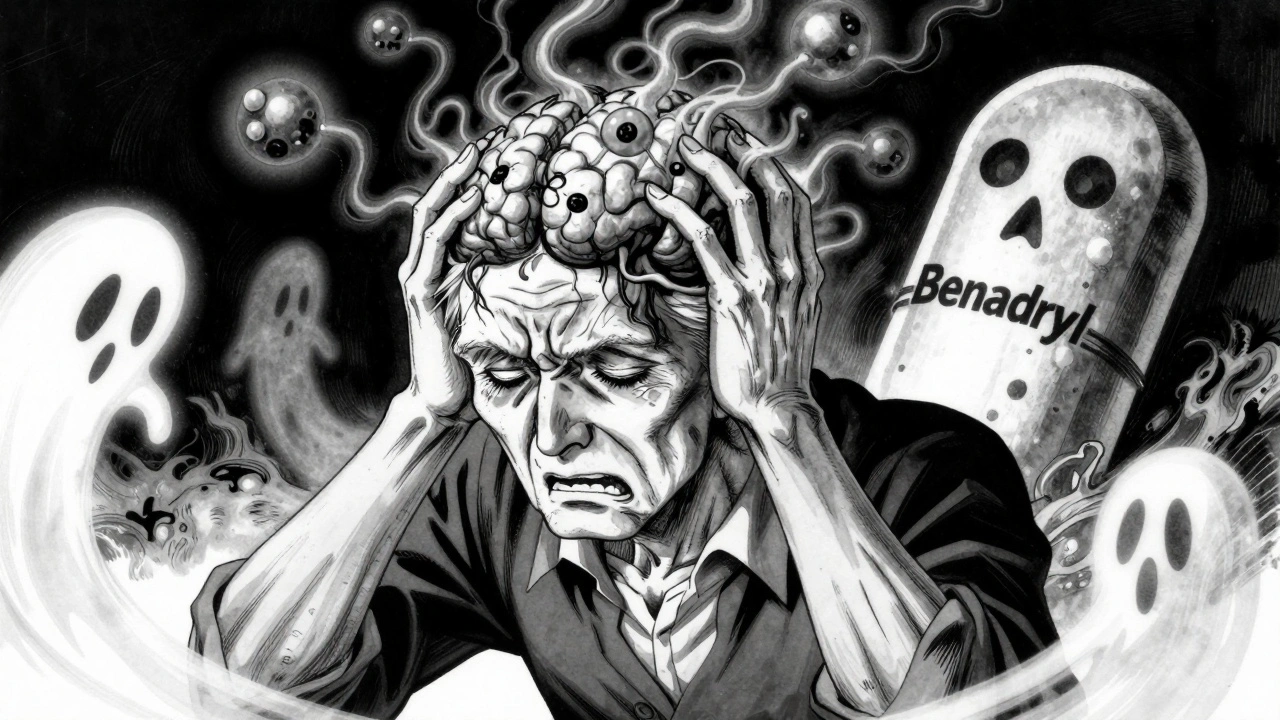
H1 blockers are your go-to for allergic reactions. They stop histamine from binding to receptors in your skin, nose, throat, and lungs. That’s why they help with runny nose, hives, watery eyes, and itching. First-generation H1 blockers like diphenhydramine (Benadryl) were developed in the 1940s. They work fast-often within 15 to 30 minutes-but they cross into your brain. That’s why you feel sleepy. Studies show 30% to 50% of users get drowsy. That’s not just a nuisance. For older adults, it raises the risk of falls by up to 50%, which is why the American Geriatrics Society warns against using them in people over 65.
Second- and third-generation H1 blockers like loratadine (Claritin), fexofenadine (Allegra), and cetirizine (Zyrtec) were made to fix that problem. They barely enter the brain. Drowsiness drops to 10% to 15%. They last 24 hours, so you take one pill a day. That’s why 68% of allergy sufferers on Reddit prefer them for daily use. They’re also safer for drivers, students, and people who need to stay alert.
What H2 Blockers Actually Do
H2 blockers don’t touch allergies. They go straight to your stomach. Histamine triggers acid production in the parietal cells. H2 blockers like famotidine (Pepcid) and cimetidine (Tagamet) block those receptors. That cuts acid by 70% to 85% for up to 12 hours. They’re used for GERD, peptic ulcers, and heartburn. You take them 30 to 60 minutes before meals to prevent acid from flaring up.
They’re not as strong as proton pump inhibitors (PPIs), which block acid at the source. But H2 blockers kick in faster-within 30 to 90 minutes. That’s why some people use them for sudden heartburn, especially if they can’t take PPIs. Famotidine is still used in hospitals for anesthesia prep because it reduces the risk of stomach acid entering the lungs during surgery. The American Society of Anesthesiologists still lists cimetidine as the gold standard for that.
Side Effects: H1 vs H2
The side effects are where these two classes really split apart.
With H1 blockers, especially the first-gen ones, you’re likely to get:
- Drowsiness (30-50% with diphenhydramine)
- Dry mouth (25% of users)
- Blurred vision (15%)
- Constipation or trouble peeing (5-10%)
These are all anticholinergic effects-meaning they mess with your nervous system’s ability to control bodily functions. That’s why older adults get confused or delirious. Caregivers on CareDash report 12% of elderly users experience mental fogginess after taking Benadryl.
H2 blockers have a different profile:
- Headache (12%)
- Dizziness (8%)
- Diarrhea or constipation (10-15%)
- Low energy or fatigue
They’re less likely to cause dry mouth or blurred vision. But cimetidine has a big problem: it interferes with liver enzymes that break down other drugs. It can affect up to 40% of common medications, including blood thinners, antidepressants, and seizure drugs. That’s why doctors avoid it now. Famotidine doesn’t have that issue, which is why it’s the H2 blocker most people use today.

When to Use Each One
Here’s the simple rule:
- Use an H1 blocker if you’re sneezing, itchy, or breaking out in hives.
- Use an H2 blocker if you’re burning in your chest after eating.
Don’t mix them up. Taking Benadryl for heartburn won’t help. Taking Pepcid for a pollen allergy won’t touch your symptoms. They’re not interchangeable.
For chronic allergies, second-gen H1 blockers are the standard. No need to risk drowsiness or cognitive decline. For occasional heartburn, famotidine works well. If you need long-term acid control, PPIs are stronger-but H2 blockers are safer over years. PPIs have been linked to kidney issues and low magnesium with long-term use. H2 blockers don’t carry those risks.
Special Cases and Warnings
There are a few gray areas.
Some people take first-gen H1 blockers like diphenhydramine on purpose for sleep. It works-but it’s not a good long-term solution. Your body gets used to it, and you wake up groggy. A 2023 GoodRx survey found 38% of users felt like they had a “morning hangover.” That’s not restful sleep.
Cardiac concerns are emerging. New research in PMC (2024) shows H2 blockers might actually help in heart failure by blocking harmful effects on heart muscle. At the same time, some H1 blockers-especially in high doses-can cause QT prolongation, a heart rhythm issue. The FDA issued warnings about this with certain antihistamines like astemizole and terfenadine, which were pulled from the market. Today’s second-gen options like loratadine and fexofenadine are considered safe at normal doses.
And then there’s ranitidine (Zantac). It was the top H2 blocker for years-until 2020, when the FDA pulled it because it contained NDMA, a probable cancer-causing chemical. That’s why you don’t see Zantac on shelves anymore. Famotidine replaced it as the go-to H2 blocker.

Real-Life Success Stories
A 42-year-old woman in Melbourne had chronic hives for three years. She tried three different H1 blockers with no luck. Then she started bilastine-a newer third-gen antihistamine approved in 2021. Within two weeks, her skin cleared. No drowsiness. No side effects. A case study in the Journal of Clinical Medicine called it a “complete resolution.”
A 68-year-old man with severe GERD couldn’t tolerate PPIs due to stomach cramps. His doctor switched him to famotidine. He took it 30 minutes before dinner. His heartburn dropped from 5 nights a week to 1. He’s been on it for 18 months with no issues.
These aren’t rare cases. They’re common outcomes when people use the right blocker for the right problem.
What’s Changing in 2025
The H1 blocker market is growing. Allergies are rising-30% of adults and 40% of kids in the U.S. now have them. New drugs like bilastine and desloratadine are being adopted because they’re even more selective. They don’t touch the brain. They don’t interfere with other drugs. They last 24 hours. Sales are expected to grow 5.2% a year through 2028.
H2 blockers are stable but shrinking. PPIs dominate the acid-reduction market. But H2 blockers still have a place. They’re cheaper. They’re safer for long-term use. And for people who need quick relief before a meal, they’re still the fastest option.
There’s also new research into combining H1 and H2 blockers for mast cell disorders and heart failure. Clinical trials are underway. It’s early, but it could mean one pill that does two jobs down the road.
For now, stick with the basics. Know your symptoms. Pick the right blocker. Don’t use an allergy pill for heartburn. Don’t use a stomach pill for a rash. And if you’re over 65, avoid first-gen H1 blockers entirely. Your brain and balance will thank you.
Can I take H1 and H2 blockers together?
Yes, but only under medical supervision. Some doctors prescribe both for severe allergic reactions or mast cell disorders. For example, a patient with chronic hives and acid reflux might take loratadine for the skin and famotidine for the stomach. But combining them without a reason can increase side effects like dizziness or fatigue. Never mix them just because you feel like it.
Is famotidine safer than omeprazole for long-term use?
Famotidine is generally safer for long-term use than omeprazole. Long-term PPI use has been linked to kidney problems, low magnesium, bone fractures, and gut infections. Famotidine doesn’t carry those risks. It’s not as strong, but if you only need moderate acid control-like occasional heartburn or nighttime reflux-it’s a better choice for staying on it for years.
Why was Zantac taken off the market?
Ranitidine (Zantac) was removed in 2020 because testing found it contained NDMA, a chemical that can cause cancer in high doses. Even though the levels were low, regulators couldn’t guarantee safety over time. All ranitidine products were pulled globally. Famotidine (Pepcid) is now the standard H2 blocker because it doesn’t have this issue.
Do H1 blockers help with asthma?
H1 blockers can help with allergy-triggered asthma symptoms like wheezing or coughing, but they don’t replace inhalers. A 1981 study showed H1 blockers reduced bronchoconstriction in asthmatic patients, but they’re not fast enough for acute attacks. Epinephrine is still the first-line treatment for asthma emergencies. H1 blockers are useful for prevention, not rescue.
Can I use diphenhydramine as a sleep aid every night?
No. While diphenhydramine makes you sleepy, it’s not designed for sleep. It disrupts natural sleep cycles, causes next-day grogginess, and increases fall risk in older adults. Over time, your body builds tolerance, so you need more to feel the same effect. There are far safer, non-habit-forming sleep aids if you need them regularly.

Webster Bull
December 12, 2025 AT 19:28h1 blockers for allergies, h2 for heartburn. dont mix em. simple as that. i used benadryl for acid once. woke up feeling like a zombie and my stomach still burned. dumb.
sharon soila
December 12, 2025 AT 22:18Thank you for this clear, evidence-based breakdown. Many people confuse these medications, and the consequences can be serious-especially for older adults. I’ve seen patients take diphenhydramine for sleep and then fall in the night. It’s preventable with better education.
Casey Mellish
December 13, 2025 AT 02:40As an Aussie who’s had to explain this to mates at the bar, I’m glad someone nailed it. We’ve got the same meds here, same risks. My uncle took Zantac for years until it vanished-no one told him why. Now he’s on famotidine and doesn’t even know the difference. Just glad he’s still breathing.
Tyrone Marshall
December 13, 2025 AT 13:13This is exactly the kind of info we need more of. Too many people treat meds like candy. I used to take Benadryl for sleep too-until I realized I wasn’t sleeping, I was just unconscious. Second-gen H1 blockers changed my life. No grogginess, no brain fog. Just calm, clear days.
Also, famotidine before pizza? Best life hack. No more midnight heartburn. And no PPIs means no weird gut bugs or kidney stress. Smart choice.
Sheldon Bird
December 15, 2025 AT 03:17Big thanks for this! I’ve been using loratadine for years and never knew why it didn’t knock me out like Benadryl. Now it makes sense 😊 Also, my grandma switched from Zantac to Pepcid after the recall-she’s been fine since. Glad someone’s keeping it real about meds.
nina nakamura
December 16, 2025 AT 11:30Anyone who takes H1 blockers for sleep is just lazy. Your body isn’t broken it’s just weak. And yes famotidine is safer than PPIs but that doesn’t mean it’s harmless. Everything has tradeoffs. Stop pretending meds are safe if you’re not a doctor.
Willie Onst
December 16, 2025 AT 23:03Love how you broke this down. I’m 31 and used to take Benadryl for allergies and sleep. Now I take Allegra and actually feel awake. It’s wild how much better life is when you stop poisoning yourself with old-school meds.
Also, famotidine before spicy food? Game changer. My stomach used to scream. Now it just gives me a thumbs up 👍
Tom Zerkoff
December 17, 2025 AT 16:28The scientific rigor in this post is commendable. The differentiation between H1 and H2 receptor pharmacology is not only accurate but pedagogically essential. One must emphasize that the anticholinergic burden of first-generation H1 antagonists is particularly deleterious in geriatric populations, as corroborated by the Beers Criteria. Furthermore, the pharmacokinetic profile of famotidine-lacking CYP450 inhibition-renders it superior to cimetidine in polypharmacy contexts. The emerging research on H2 blockade in heart failure pathophysiology warrants further investigation, as it may represent a paradigm shift in cardioprotective pharmacotherapy.
It is also noteworthy that the global prevalence of allergic diseases has increased by 2.3% annually since 2015, reinforcing the necessity for selective, non-sedating antihistamines in public health strategy. The withdrawal of ranitidine was a necessary regulatory action, as NDMA is a Class 2A carcinogen per IARC guidelines. The substitution with famotidine exemplifies evidence-based pharmaceutical stewardship.
Scott Butler
December 18, 2025 AT 19:34Who funded this? Big Pharma loves pushing expensive second-gen antihistamines while hiding how dangerous PPIs are. You think famotidine is safe? What about the 2022 study linking it to liver enzyme spikes? And why did the FDA let them replace Zantac with the same chemical structure? They’re just swapping one poison for another. Wake up.
Ronan Lansbury
December 19, 2025 AT 22:08Of course the FDA pulled Zantac. They’ve been hiding the truth about histamine and brain chemistry for decades. H2 blockers don’t just reduce acid-they interfere with the pineal gland’s melatonin production. That’s why everyone’s tired. That’s why kids are anxious. That’s why we’re all just walking zombies on Pepcid. Wake up. The real cure is fasting and sunlight.
Karen Mccullouch
December 21, 2025 AT 05:36Wow so you're telling me I've been taking Benadryl for my hives and not my heartburn? What a joke. Everyone knows you just take whatever makes you sleepy. My mom takes 3 Benadryl every night and says she feels 'reset'. You're just mad because you don't have the guts to take real medicine. 🤡
Michael Gardner
December 21, 2025 AT 06:17Wait, so H1 blockers don’t help with asthma? But I’ve seen people use them for wheezing. And what about that 2023 study showing cetirizine reduced nighttime cough in kids? You’re oversimplifying. And why is famotidine ‘safer’ if it’s still linked to vitamin B12 deficiency? You left out half the story.
Also, why is everyone acting like second-gen antihistamines are magic? They still cause dry mouth, fatigue, and some people report weird dreams. This feels like a corporate PR piece.