When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck. It’s because of CGMP - Current Good Manufacturing Practices - enforced by the FDA. These aren’t suggestions. They’re legally binding rules that every generic drug maker, whether in Ohio or India, must follow to sell medicine in the U.S.
What CGMP Actually Means for Generic Drugs
CGMP stands for Current Good Manufacturing Practices. The "current" part is critical. It means manufacturers can’t rely on old methods. They must use up-to-date technology, equipment, and processes. The FDA doesn’t care if you’ve been making the same pill for 20 years. If your process isn’t validated, your records aren’t complete, or your lab isn’t clean, your product is considered adulterated - and illegal to sell. The rules are laid out in 21 CFR Parts 210 and 211. These aren’t vague guidelines. They’re specific. For example:- Every batch of raw material must be tested before use (§ 211.84).
- Equipment must be cleaned, calibrated, and logged - every time.
- Personnel must be trained, documented, and qualified for their roles.
- Environmental controls must prevent contamination - air quality, humidity, even employee clothing matter.
- Stability testing must prove the drug stays potent and safe until its expiration date.
Why the Same Rules Apply to Generics and Brand Drugs
Many people think generics are "cheaper because they’re lower quality." That’s false. The FDA requires generic manufacturers to meet the exact same standards as brand-name companies. Pfizer, Merck, and a small generic lab in Tennessee all follow the same 21 CFR Part 211 rules. This isn’t just policy - it’s science. A generic drug must deliver the same amount of active ingredient into the bloodstream at the same rate as the brand. That’s called bioequivalence. But bioequivalence means nothing if the manufacturing process is sloppy. A pill might pass a lab test but still be unsafe if it’s contaminated or degrades too fast on the shelf. The FDA reviews every single Abbreviated New Drug Application (ANDA) for compliance with CGMP before approving a generic. No CGMP compliance? No approval. Period.Key Areas the FDA Inspects Most
Not all parts of CGMP are inspected equally. Based on FDA enforcement data from 2022, these are the top violation areas:- Laboratory Controls (§ 211.160) - 22% of violations. This includes inaccurate testing, missing data, or failing to validate test methods.
- Production and Process Controls (§ 211.100) - 19% of violations. Missing in-process checks, unvalidated processes, or not documenting deviations.
- Data Integrity (21 CFR Part 11) - 63% of warning letters to foreign facilities involve this. Spurious records, deleted logs, or bypassing audit trails.
- Equipment Cleaning Validation - Swab tests must show no more than 100 CFU (colony-forming units) of microbes. Many companies fail because they don’t test thoroughly enough.

How Companies Actually Implement CGMP
Getting CGMP right isn’t easy. It takes time, money, and expertise. For a mid-sized generic manufacturer, annual compliance costs average $2.3 million. That’s not profit - that’s overhead. It covers:- Electronic quality management systems (eQMS)
- Staff training (80-120 hours per person per year)
- Facility qualification (IQ/OQ/PQ)
- Process validation (typically 3 consecutive batches)
- Regular audits and inspections
Foreign vs. Domestic Facilities - The Enforcement Gap
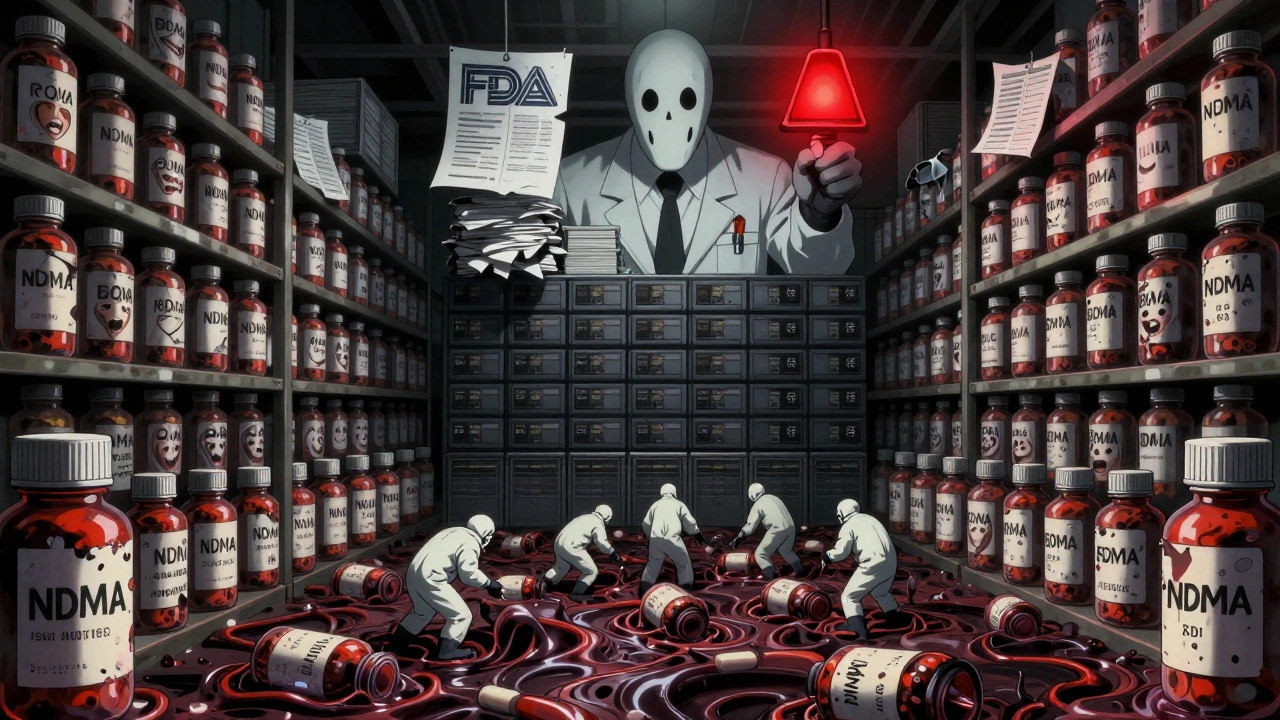
The FDA inspects over 1,800 foreign manufacturing sites and 127 U.S. ones. But here’s the problem: foreign sites get 43% fewer warning letters per inspection than U.S. sites, according to FDA data from 2020-2022. That doesn’t mean foreign plants are better. It means inspection frequency and enforcement are uneven. Harvard Medical School’s Aaron Kesselheim called this a "critical flaw" in the system. The FDA admits it - and is fixing it. Their 2023-2027 plan allocates 25% more resources to foreign inspections. India and Europe supply most of the world’s generic drugs. But when a contamination happens - like the 2022 Pakistan metformin deaths linked to diethylene glycol - the FDA responds fast. In May 2023, they issued an immediate guidance requiring testing for toxic contaminants in high-risk ingredients like glycerin and sorbitol. That wasn’t a suggestion. It was a new rule, effective immediately.What’s Changing in CGMP - and Why It Matters
CGMP isn’t static. The FDA is pushing for modernization:- Continuous Manufacturing - Instead of making drugs in batches, some companies now run a constant flow. Teva reduced batch failures from 4.2% to 0.7% using this method. But traditional CGMP was built for batch processing. New guidance is coming in 2024 to adapt the rules.
- Data Integrity - Expect tighter Part 11 enforcement in 2024. 73% of industry leaders say it’s the top regulatory concern.
- Supply Chain Security - The Drug Supply Chain Security Act is forcing stricter tracking of active ingredients. 68% of manufacturers expect tougher component testing soon.
- AI and Predictive Quality - McKinsey predicts 65% of manufacturers will use AI to predict quality failures by 2028. Think real-time sensors, machine learning on production data - not just paper logs.
What Happens If You Fail?
Failing CGMP isn’t a slap on the wrist. Consequences include:- Warning letters - public, posted on the FDA website.
- Import alerts - your drugs get blocked at U.S. ports.
- Consent decrees - court orders forcing you to fix everything under court supervision.
- Civil penalties - up to $1 million per violation.
- Product recalls - costly, damaging, and sometimes deadly.
How to Get Started With CGMP Compliance
If you’re starting a generic drug operation, here’s the real-world path:- Build a Quality Management System (QMS) with written procedures for every step.
- Qualify your facility - Install, Operate, and Performance qualify all equipment.
- Validate your processes - Run 3 consecutive batches with full documentation.
- Train your team - 80-120 hours per year per employee.
- Implement eQMS - 65% of large firms use it by 2023. Paper records won’t cut it.
- Prepare for FDA inspection - Expect a 2-5 day audit. They’ll review every log, every test, every signature.
Final Reality Check
CGMP for generics isn’t about perfection. It’s about control. It’s about knowing what went into your drug, how it was made, and how you know it’s safe. It’s not glamorous. It’s paperwork, swab tests, calibration logs, and audit trails. But it’s what keeps you from getting a contaminated pill. It’s why a $2 generic blood pressure pill works just as well as the $100 brand name. And it’s why the FDA will keep tightening the rules - because patient safety isn’t negotiable.As FDA Commissioner Robert Califf said in 2023: "CGMP provides for systems that assure proper design, monitoring, and control of manufacturing processes and facilities." That’s the only standard that matters.
Are generic drugs held to the same manufacturing standards as brand-name drugs?
Yes. The FDA requires generic drugs to be manufactured under the exact same Current Good Manufacturing Practices (CGMP) as brand-name drugs. This is non-negotiable. The FDA reviews manufacturing processes for every generic drug application, and failure to meet CGMP results in denial of approval or product recalls.
What happens if a generic drug manufacturer violates CGMP rules?
Violations can lead to warning letters, import alerts, consent decrees, civil penalties up to $1 million per violation, or full product recalls. The FDA publishes warning letters publicly. Companies may be barred from selling drugs in the U.S. until they fix the issues under FDA supervision.
Do foreign generic manufacturers follow the same CGMP rules as U.S. ones?
Yes, legally. All manufacturers, regardless of location, must comply with U.S. CGMP to sell drugs in America. However, enforcement has been uneven - foreign facilities historically received fewer warning letters per inspection than U.S. sites. The FDA is now increasing foreign inspection resources to close this gap.
How often does the FDA inspect generic drug factories?
Domestic facilities are inspected about every 18-24 months on average, with some getting inspected more frequently based on risk. Foreign facilities are inspected less often, though the FDA is increasing inspections by 25% through 2027. High-risk or previously non-compliant sites may be inspected annually.
What are the biggest challenges for small generic manufacturers with CGMP?
Small manufacturers struggle most with cost and complexity. Compliance can cost $2.3 million annually for mid-sized firms. Key challenges include implementing electronic records (21 CFR Part 11), training staff, validating processes, and dealing with inconsistent FDA inspector interpretations. Many lack the resources of big pharma, making compliance a major financial burden.
Is CGMP going to change in the next few years?
Yes. The FDA is moving toward real-time quality control using AI, continuous manufacturing, and predictive analytics. Expect stricter rules on data integrity, supply chain tracking, and testing for emerging contaminants like ethylene glycol. The 2024 draft guidance on continuous manufacturing will be a major shift away from traditional batch-based validation.


James Kerr
December 3, 2025 AT 11:31Albert Essel
December 4, 2025 AT 20:54Charles Moore
December 5, 2025 AT 13:29Gavin Boyne
December 7, 2025 AT 03:26Rashi Taliyan
December 7, 2025 AT 06:18Kara Bysterbusch
December 7, 2025 AT 14:10Rashmin Patel
December 7, 2025 AT 21:42sagar bhute
December 9, 2025 AT 13:45Cindy Lopez
December 10, 2025 AT 11:46shalini vaishnav
December 10, 2025 AT 20:26vinoth kumar
December 12, 2025 AT 14:24bobby chandra
December 14, 2025 AT 02:32