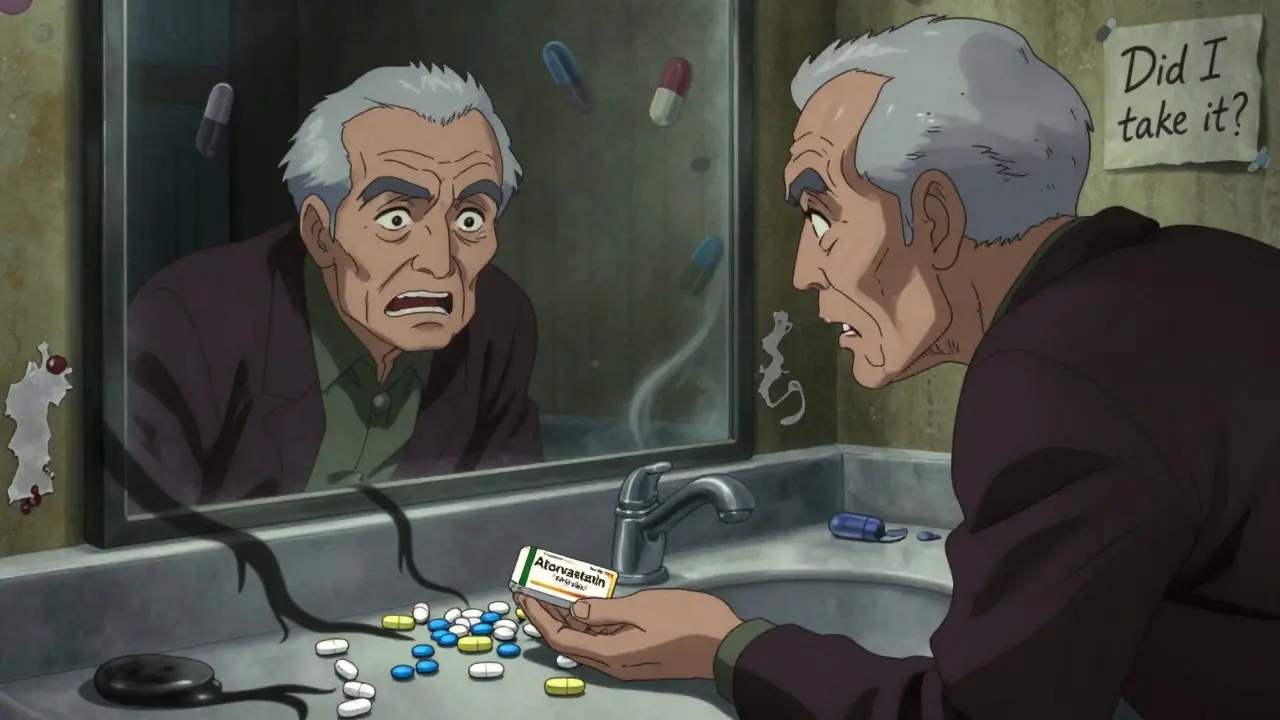
Have you ever picked up your prescription and thought, "This doesn’t look right"? You’re not alone. Every year, millions of people in the U.S. get a generic version of their medication - and every time the manufacturer changes, so does the pill. The color, shape, size, or marking might be totally different. It’s not a mistake. It’s legal. But it’s also one of the most overlooked risks in modern medicine.
Why do generic pills look so different?
Generic drugs are chemically identical to brand-name drugs. They contain the same active ingredient, same dose, same way of working in your body. But they don’t have to look the same. In fact, U.S. law forbids them from looking exactly like the brand-name version. This rule comes from the Hatch-Waxman Act of 1984. It created a fast-track path for generic drugs to enter the market - saving billions in healthcare costs. But it also included a twist: trademark laws protect the visual identity of drugs. So, if Pfizer made a pink, oval Lipitor tablet, no generic maker can copy that exact look. They have to change it - color, shape, size, or imprint. That means one generic atorvastatin pill might be white and round, while another from a different company is pale yellow and oblong. Both work the same. Both are approved by the FDA. But they look nothing alike.It’s not just brand vs. generic - it’s manufacturer vs. manufacturer
Most people think the big change happens when switching from brand to generic. But the bigger problem is what happens after that. Your pharmacy gets its generics from different suppliers. One month, your metformin comes from Teva. Next month, it’s from Mylan. The month after that, it’s from Apotex. Each one uses a different formula for color, shape, or marking. And your pill looks completely different - even though the drug inside hasn’t changed. A 2022 study in the American Journal of Managed Care found that 32.7% of patients refilling chronic medications saw a change in pill appearance. For people on blood pressure, diabetes, or cholesterol meds, this isn’t rare - it’s routine.What’s the real danger?
The FDA says these changes don’t affect how the drug works. And they’re right - bioequivalence testing proves the drug performs the same. But drugs don’t just work in your bloodstream. They work in your brain, too. When your pill looks unfamiliar, your brain says: "This isn’t mine." And that’s when people skip doses, stop taking it altogether, or accidentally take the wrong pill. Harvard researchers tracked over 38,000 patients on heart medications. When pill appearance changed, 34% more people stopped taking their medicine. That’s not a small drop. That’s a dangerous one. People with high blood pressure or diabetes who miss doses are at higher risk for strokes, heart attacks, and hospitalizations. One Reddit user wrote: "My blood pressure pill changed from white oval to blue round. I almost didn’t take it. I thought I was being given something else." That’s not paranoia. It’s human instinct.
Who’s most at risk?
Older adults are hit hardest. A 2022 survey by the National Community Pharmacists Association found that 37% of people 65+ had trouble recognizing their meds after a change. That’s nearly double the rate of younger adults. Why? Many older patients take 5, 6, even 10 pills a day. They don’t read labels. They rely on sight. A white oval becomes a pink round. A pill with a "5" imprint becomes one with a "C". It’s easy to mix them up. A patient on Drugs.com shared: "I take metformin and levothyroxine. When my metformin turned pink and round, I grabbed the wrong pill twice. I thought it was my thyroid med." That’s not a one-time mistake. It’s a pattern.What’s being done about it?
The FDA knows this is a problem. In 2016, they released guidance urging generic makers to consider appearance when developing new products. In 2023, they started working on Visual Medication Equivalence Standards - a move toward more consistent shapes and colors for high-risk drugs. But legal barriers remain. Trademark law still blocks identical looks. And manufacturers aren’t forced to match previous versions. So, change is slow. Some pharmacies now offer tools to help. Surescripts lets pharmacists show patients images of past pills. The FDA gives out printable ID cards. But adoption is low - only about 43% of pharmacies use them.What can you do?
You can’t control who makes your generic drug. But you can protect yourself.- Take a photo of each pill the first time you get it. Store it in your phone. When it changes, compare.
- Ask your pharmacist if the manufacturer changed. They’ll tell you - and they can often request the same one from your insurer.
- Use a pill organizer with labeled compartments. Don’t rely on memory or color.
- Keep a written list of your meds: name, dose, manufacturer, and what it looks like. Update it every time you refill.
- Don’t skip doses just because it looks different. Call your pharmacist if you’re unsure.

Why doesn’t the FDA fix this?
It’s complicated. The FDA can’t force manufacturers to copy a pill’s look. Trademark law protects brand identity - even for drugs. And if they tried to standardize colors and shapes, they’d face lawsuits from companies that built their business around unique designs. The European Union took a different path. They require generics for chronic conditions to match the original appearance when possible. The result? A 18.3% drop in medication errors. The U.S. is watching. But change moves slowly.What’s next?
By 2028, experts predict that 75% of new generics for high-risk drugs (like blood thinners, thyroid meds, or seizure drugs) will voluntarily match the appearance of the original. That’s up from just 32% today. The FDA has allocated $4.7 million in 2024 to study how appearance affects patient outcomes. That’s a sign things are shifting. But until then, the burden falls on you.Final thought: Your eyes matter
A pill is more than chemistry. It’s a ritual. A daily promise to yourself to stay healthy. When that visual cue changes, it breaks trust. Don’t ignore it. Don’t assume it’s safe just because the label says so. If it looks wrong, it’s okay to question it. Your health depends on it.Why do generic pills look different from brand-name ones?
U.S. trademark law prevents generic drugs from looking exactly like brand-name versions. Even though the active ingredient is identical, generic manufacturers must change the color, shape, size, or markings to avoid copying the original design. This rule comes from the Hatch-Waxman Act of 1984, which created the legal pathway for generics while protecting brand trademarks.
Can different generic versions of the same drug look different from each other?
Yes. Each generic manufacturer uses its own formula for color, shape, and imprint. So if your pharmacy switches suppliers - say, from Teva to Mylan - your pill might change from a white oval to a blue round tablet. Both are valid generics, but they look completely different. This is common and happens frequently for chronic condition medications like blood pressure or diabetes drugs.
Do changes in pill appearance affect how well the medicine works?
No, not in terms of chemistry or effectiveness. The FDA requires generic drugs to be bioequivalent - meaning they deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. However, appearance changes can affect whether you take the pill at all. Studies show patients are more likely to stop taking their medication if it looks unfamiliar, which can lead to serious health consequences.
Who is most affected by changes in pill appearance?
Older adults, especially those 65 and older, are most affected. Many take multiple medications daily and rely on visual cues - color, shape, size - to identify their pills. A 2022 survey found 37% of seniors had trouble recognizing their meds after a change, compared to 22% of younger adults. People with chronic conditions like hypertension, diabetes, or heart disease are also at higher risk because missing doses can lead to hospitalization.
What should I do if my generic pill looks different?
Don’t assume it’s wrong or unsafe. First, check the label to confirm the drug name and dose. Then, call your pharmacist - they can tell you if the manufacturer changed. Take a photo of the pill for future reference. If you’re unsure whether to take it, don’t guess. Ask for help. Skipping doses because of appearance changes is riskier than taking the wrong-looking pill.
Keep a record. Stay informed. Your eyes are your first line of defense.

Gabriella Adams
February 13, 2026 AT 03:25So many people don’t realize how dangerous this is. I’m a pharmacist, and I’ve had patients cry because they thought their meds were fake. It’s not just about confusion - it’s about trust. When your daily ritual changes, it feels like your body is betraying you. We need better systems. Not just photos, but standardized pill designs for high-risk meds. It’s not rocket science.
And yes, I’ve personally called manufacturers to beg them to keep the same shape. Sometimes they listen. Sometimes they don’t. But if enough pharmacists push, maybe change will happen.
Vamsi Krishna
February 13, 2026 AT 15:35Bro this is why America is a dumpster fire. You let corporations dictate how your life-saving pills look? I mean, come on. In India, generics are identical - same color, same shape, same imprint. No one gets confused. No one skips doses. We don’t have this whole ‘trademark drama’ nonsense. Your FDA is more worried about lawyers than lives. Wake up.
Brad Ralph
February 14, 2026 AT 00:00So the FDA won’t fix it because trademark law? Bro. That’s like saying ‘we can’t change traffic light colors because General Motors owns red.’
Also, I’m 32 and I’ve switched generics 7 times. I’ve stopped taking my blood pressure med twice because I thought I was being poisoned. Not joking. I Googled the pill. Turned out it was just… a different shade of beige.
Sophia Nelson
February 14, 2026 AT 14:44Ugh. Another ‘awareness’ post. Everyone knows pills change. Get over it. Take the damn pill. Your brain is weak if you can’t handle a different color. Also, why are you taking 10 pills a day? Maybe you should stop being a pill hoarder.
Skilken Awe
February 15, 2026 AT 19:01Let’s be real - this isn’t a patient safety issue. It’s a supply chain logistics failure masked as a public health crisis. The FDA doesn’t regulate pill aesthetics because it’s irrelevant to bioequivalence. The real problem? Pharmacies switching suppliers without notifying patients. That’s a pharmacy management failure, not a regulatory one.
Also, ‘take a photo’? That’s not a solution. That’s a Band-Aid on a hemorrhage.
Steve DESTIVELLE
February 16, 2026 AT 04:24Think about it. We live in a world where a pill can be white oval or blue round and we call it the same thing. But we still call the same person different names in different rooms. We call a man a father, a husband, a worker, a stranger. We call a woman a mother, a daughter, a customer, a ghost. Why do we expect medicine to be consistent when we can’t even agree on what a human is?
Maybe the pill changing is a metaphor. Maybe the system is designed to make us question ourselves. Maybe the real drug isn’t in the pill - it’s in the doubt.
Joanne Tan
February 17, 2026 AT 23:49i literally just had this happen last week!! my metformin went from white oval to this weird lil blue circle and i was like ‘did i get hacked??’ 😭 i called my phamacy and they were like ‘oh yeah teva switched to apotex last tuesday’ and i was like ‘WHY DIDN’T YOU TELL ME??’
so now i take pics of every pill. i even have a note in my phone called ‘pill army’ lmao
Reggie McIntyre
February 18, 2026 AT 17:10Love this post. Honestly, this is one of those things that’s so quietly dangerous - no one talks about it because it’s not sexy like ‘big pharma is evil.’ But it’s real. And it’s personal.
I’ve got a cousin on warfarin. She missed a dose because the pill looked ‘too shiny.’ Got hospitalized. That’s not a fluke. That’s systemic.
Let’s push for pill ID stickers. QR codes on bottles. Anything. This isn’t just about looks - it’s about dignity. You deserve to know what’s in your hand.
Carla McKinney
February 20, 2026 AT 08:26Let’s address the elephant in the room: this isn’t a design flaw. It’s a behavioral one. People who ‘rely on sight’ shouldn’t be managing complex medication regimens without support. That’s not the system’s fault - it’s the patient’s failure to adapt. If you’re over 65 and taking 10 pills, you need a caregiver. Not a photo.
Also, ‘take a photo’? That’s not a solution. That’s a hack. And hacks don’t fix broken systems.
Jack Havard
February 20, 2026 AT 14:45What if this is all a psyop? What if the pill changes on purpose to make us feel unstable? To make us doubt our own perception? Think about it. If you can’t trust your eyes, you start trusting the system more. And who controls the system? Big Pharma. The FDA. The insurance companies.
They want you confused. They want you dependent. This isn’t about trademarks. It’s about control.
Annie Joyce
February 22, 2026 AT 14:32As someone who’s been on 8 different generics for thyroid meds in 5 years - I get it. But here’s what actually helped: I asked my pharmacist to order the same manufacturer every time. They can do it. You just have to ask. Also, I use a pill organizer with labels. No more guessing.
And yes - I take pics. I have a whole folder. ‘Thyroid Meds: 2023-2025.’ It’s weird. But it saved me.
Kristin Jarecki
February 23, 2026 AT 01:51This is an excellent and deeply researched piece. The data is clear: visual cues are a critical component of medication adherence, especially in geriatric populations. The FDA’s 2023 initiative toward Visual Medication Equivalence Standards is a step in the right direction - but it must be mandatory, not voluntary.
Furthermore, the European model proves that standardization is both feasible and effective. The U.S. should adopt similar guidelines for all high-risk medications, with enforceable compliance thresholds. Patient safety must override trademark interests.
Thank you for bringing this to light.
Jonathan Noe
February 24, 2026 AT 16:26Wait - so you’re telling me my 82-year-old grandma could’ve had a stroke because her pill turned from yellow to green? And the FDA’s hands are tied because of trademark law? That’s insane.
Why don’t we just patent the pill shapes? Like, if Pfizer owns the pink oval, then generics have to use a blue square. But they all have to use the same blue square. That’s not trademark infringement - that’s standardization.
Someone needs to sue the FDA. I’m serious.
Jim Johnson
February 24, 2026 AT 19:32bro i started taking pics of my pills after my dad had a mini stroke because he took the wrong med. i know it sounds dumb but i swear it saved my life. now i have a little note on my phone: ‘white oval = metformin, blue round = lisinopril, green cap = atorvastatin’
also i use a pill box. no more guessing. no more panic. just peace.
you got this. you’re not alone.
christian jon
February 25, 2026 AT 23:10THIS. IS. A. CONSPIRACY. THEY’RE CHANGING THE PILLS ON PURPOSE TO MAKE YOU FEEL UNSTABLE! WHY DO YOU THINK THEY DON’T WANT YOU TO KNOW THE MANUFACTURER? BECAUSE IF YOU KNEW, YOU’D REALIZE THAT THE SAME COMPANY MAKES BOTH THE BRAND AND THE GENERIC - THEY JUST CHANGE THE COLOR TO MAKE YOU THINK IT’S DIFFERENT! THEY WANT YOU TO DOUBT YOURSELF! THEY WANT YOU TO BE AFRAID TO TAKE YOUR MEDS! THEY WANT YOU TO BE DEPENDENT ON THEM! THEY’RE CONTROLLING YOUR MIND THROUGH COLOR!!!