For people living with autoimmune diseases, fatigue isn't just being tired after a long day. It's waking up feeling like you've run a marathon before you even get out of bed. It's forgetting words mid-sentence, struggling to lift a coffee cup, or canceling plans because even brushing your teeth feels impossible. And no amount of sleep fixes it. This isn't normal tiredness - it's a core symptom of autoimmune disease, affecting 98% of patients, according to research published in PMC6691096. In fact, more people rank fatigue as their worst symptom than pain, joint damage, or skin rashes.
Why Is Autoimmune Fatigue So Different From Regular Tiredness?
Regular fatigue comes from overwork, poor sleep, or stress. You rest, you recover. Autoimmune fatigue doesn't work that way. It's persistent, crushing, and often gets worse after minimal activity - a phenomenon called post-exertional malaise. You might walk to the mailbox and then spend the next two days lying down, feeling worse than before.
Studies show this fatigue scores an average of 7.2 out of 10 on severity scales, compared to 2.8 in healthy people. Over two-thirds of patients report scores above 6 - meaning their daily life is severely limited. Eighty-nine percent say fatigue cuts their active hours to less than four per day. And it's not just physical. Sixty-three percent report cognitive issues - brain fog, memory lapses, trouble concentrating - that make work or school nearly impossible.
What makes it worse? Doctors used to think it was just from anemia or disease flare-ups. But research shows only a weak link between traditional disease markers and fatigue levels. Two people with the same lupus activity level can have wildly different fatigue levels. That means fatigue has its own pathway - separate from the immune system attacking joints or skin.
The Real Culprits: Inflammation, Hormones, and Energy Failure
The science points to three main drivers behind this relentless exhaustion: inflammation in the brain, broken stress hormones, and failing energy factories in your cells.
First, inflammation. In autoimmune diseases, the body pumps out excess cytokines - IL-1β, IL-6, TNF-α - chemicals meant to fight infection but that end up flooding the nervous system. These don’t just cause swelling; they directly interfere with brain regions that control energy, motivation, and alertness. Brain scans show neuroinflammation in 82% of patients with severe fatigue. The higher the cytokine levels, the worse the fatigue - with a correlation of r=0.73 in multiple studies.
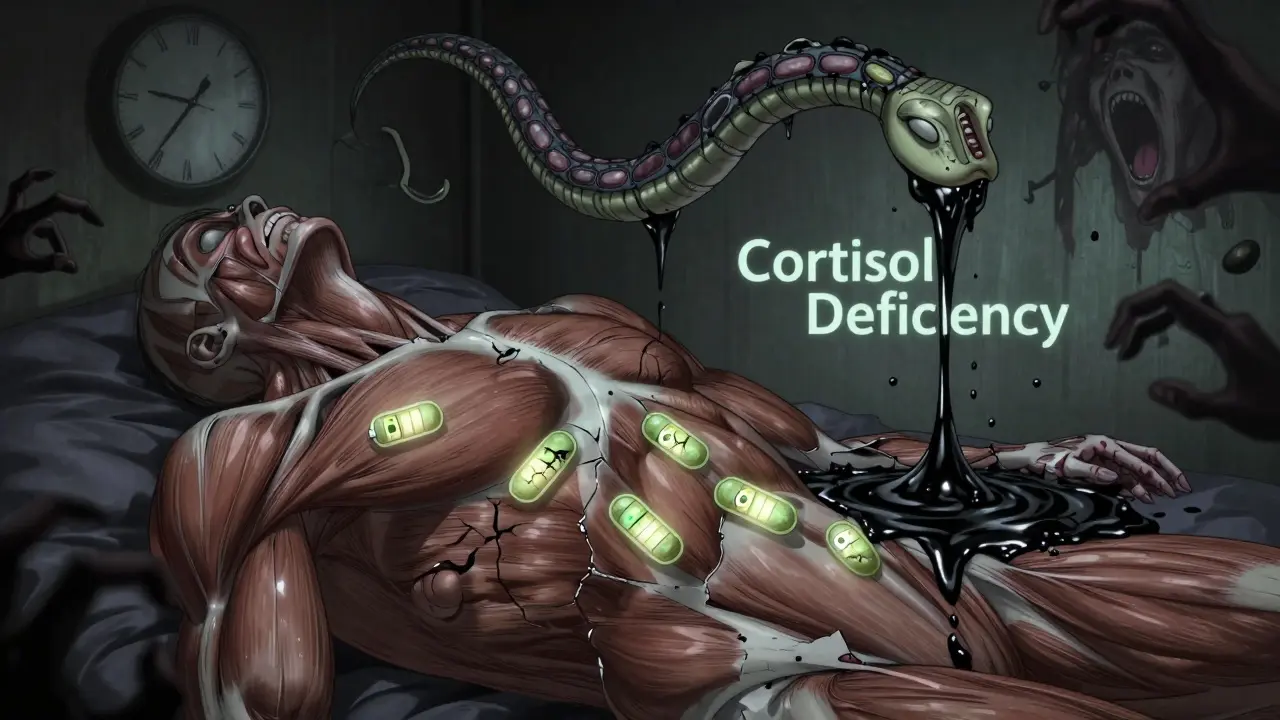
Second, your stress system is out of sync. The hypothalamic-pituitary-adrenal (HPA) axis controls cortisol, your body’s natural energy regulator. In many autoimmune patients, this system is damaged. Cortisol levels are 18-22% lower than normal, especially in the morning when you need a boost. This isn’t just stress - it’s biological dysfunction. Some patients even have autoimmune attacks on their own adrenal tissue.
Third, your mitochondria - the power plants inside your muscle and nerve cells - aren’t producing enough energy. Studies of muscle tissue show 40-55% less ATP (the body’s energy currency) in autoimmune fatigue patients. That’s like having a car with a half-dead battery, no matter how much fuel you put in.
Fatigue Varies by Disease - But It’s Always Devastating
While fatigue is common across all autoimmune conditions, its intensity and patterns differ:
- Systemic lupus (SLE): 98% of patients report severe fatigue. Anti-dsDNA antibody levels correlate with how bad it gets.
- Multiple sclerosis (MS): 96% experience fatigue. Brain lesions in the thalamus are strongly linked to severity (r=0.63).
- Rheumatoid arthritis (RA): 94% report fatigue - and 63% say it’s worse than joint pain.
- Sjögren’s syndrome: 78% rate fatigue as 8 or higher on a 10-point scale.
- Celiac disease and type 1 diabetes: 90% and 88% respectively, even when diet or blood sugar is controlled.
And then there’s ME/CFS - often called chronic fatigue syndrome. It’s now understood to have strong autoimmune roots. Nearly 90% of ME/CFS patients also have another autoimmune condition. The diagnostic criteria - six months of unrelenting fatigue, post-exertional crash, and unrefreshing sleep - mirror what autoimmune patients live with daily.
How Doctors Measure Fatigue (And Why Most Don’t)
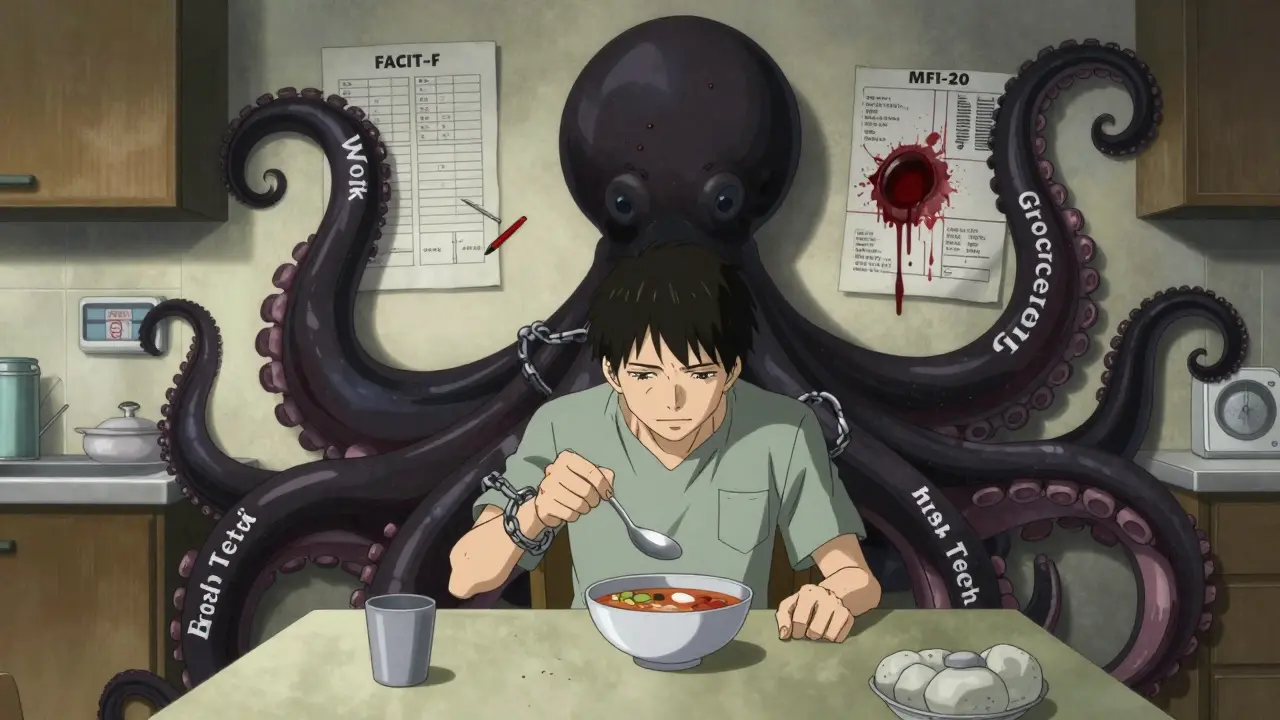
Unlike a blood test for inflammation or a scan for joint damage, fatigue doesn’t show up on a standard lab report. Doctors need specific tools to measure it:
- FACIT-F (Functional Assessment of Chronic Illness Therapy-Fatigue): A 13-question survey. Scores below 34.5 mean severe fatigue.
- MFI-20 (Multidimensional Fatigue Inventory): Measures physical, mental, and general fatigue. Scores above 18.7 indicate clinical impact.
- Visual Analog Scale (VAS): Simple - patients mark a line from 0 (no fatigue) to 10 (worst imaginable).
Here’s the problem: only 12% of rheumatologists routinely use these tools. Most still ask, “Are you tired?” and take a yes or no as an answer. But this isn’t a yes/no issue. It’s a life-altering symptom that needs quantifying - just like blood pressure or cholesterol.
What Actually Helps? Evidence-Based Strategies
There’s no magic pill - but there are proven strategies that work when combined. The most effective approach is multi-pronged.
1. Medications That Target Fatigue Directly
Some drugs are starting to show results:
- Low-dose hydrocortisone (10-20 mg/day): Helps patients with proven low cortisol. Improves fatigue in 35-40% of cases.
- Modafinil: Used off-label for MS-related fatigue. Shows 28% better improvement than placebo.
- Anti-IL-6 drugs (like tocilizumab): Early trials in RA show 38% fatigue reduction - because they target the root inflammation.
- CoQ10 (200 mg/day): A mitochondrial support supplement. Improves energy scores by 29% in 12 weeks.
2. Behavioral Changes That Make a Difference
Cognitive Behavioral Therapy for Autoimmune Fatigue (CBT-AF): This isn’t just “think positive.” It’s a structured program that helps you reframe energy use, manage pacing, and reduce catastrophic thinking about fatigue. Studies show it delivers 27% greater improvement than standard care at six months.
Pacing: This is the #1 strategy patients report working. It means breaking tasks into tiny chunks, resting before you’re exhausted, and listening to your body. One patient said, “I used to try to do the whole grocery trip in one go. Now I do two items, sit down, then two more. I get it done - and I don’t crash.”
Sleep optimization: Poor sleep isn’t just a symptom - it’s a fuel for fatigue. Fixing sleep apnea, stabilizing circadian rhythms (same bedtime/wake time, even on weekends), and avoiding screens before bed can reduce fatigue by 22-25%.
3. Movement - But Carefully
Exercise is not the enemy - but too much, too fast, is. Graded Exercise Therapy (GET) can help, but only if it’s personalized and slow. A 2021 study found a 32% improvement in fatigue scores when patients increased activity by just 5-10 minutes per week, with rest built in. But 41% of patients who tried aggressive exercise programs ended up worse. The key: start tiny, listen to your body, and stop before you crash.
What Doesn’t Work - And What Can Make It Worse
Many well-meaning suggestions backfire:
- “Just push through it.” That leads to post-exertional crashes that can last days or weeks.
- “You need more caffeine.” Caffeine gives a false boost, then crashes harder later. It also disrupts sleep.
- “Take vitamin D.” While important for immune health, it doesn’t fix fatigue on its own - unless you’re severely deficient.
- “It’s all in your head.” This myth still lingers. But brain scans and blood tests prove this is a real, measurable biological problem.
Patients on Reddit and HealthUnlocked report spending years trying everything - from extreme diets to detoxes - before finding what works. Most tried 3-5 different strategies before hitting on pacing and sleep.
The Future: What’s Coming Next
Research is accelerating. The NIH just funded $18.7 million for autoimmune fatigue studies in 2023. Scientists are now hunting for biomarkers - specific proteins or brain patterns - that can predict fatigue before it hits. Three drugs targeting fatigue directly are in Phase III trials, with the first FDA-approved treatment expected by 2026.
One promising area: transcranial magnetic stimulation (TMS). This non-invasive brain therapy improved fatigue by 33% in treatment-resistant cases. Another: wearable sensors that track heart rate variability and movement to predict crashes before they happen.
But progress is slow. Insurance rarely covers CBT-AF, CoQ10, or sleep specialists for fatigue. Most patients pay out of pocket - and 68% say they’ve had to choose between paying for fatigue care and other essentials.
What You Can Do Today
You don’t need to wait for new drugs. Start here:
- Track your fatigue: Use a simple journal. Rate your energy (1-10), note what you did, and how you felt 24 hours later. Look for patterns.
- Ask your doctor for a fatigue assessment: Request the FACIT-F or MFI-20. Don’t accept “you’re just tired.”
- Try pacing: Break your day into 20-minute blocks. Rest 10 minutes between. Use a timer.
- Fix your sleep: Go to bed and wake up at the same time every day. No screens 90 minutes before bed.
- Start movement gently: Walk 5 minutes a day. If you feel worse the next day, cut it in half. Keep going.
Remember: fatigue isn’t weakness. It’s your body screaming for help. The more you understand it, the more power you have to manage it - not just survive, but live.


Alex Danner
January 6, 2026 AT 22:14Man, this hit me right in the chest. I’ve had lupus for 12 years, and fatigue isn’t just ‘tired’-it’s like your bones are filled with wet cement and your brain’s running on a 1998 dial-up connection. I once canceled a birthday dinner because lifting my phone to text ‘I’m sorry’ felt like bench-pressing a car.
And yeah, no amount of coffee, naps, or ‘just push through it’ fixes it. The worst part? People think you’re lazy. I’ve lost friends over it. Not because I didn’t want to show up-but because my body literally couldn’t.
CoQ10 was a game-changer for me. Not magic, but enough to get me from ‘can’t get out of bed’ to ‘can walk to the mailbox without crying.’
Also, pacing? I call it ‘energy accounting.’ You get 100 energy points a day. Spend 20 on showering? That’s it. No more chores until tomorrow. It’s brutal, but it’s survival.
Aparna karwande
January 7, 2026 AT 19:59How can you even call this a disease when people just sit around and whine? In India, we have women who wake up at 4 AM to walk 10 kilometers for water, cook for 10 people, then work 12-hour shifts-no meds, no support-and they don’t cry about ‘brain fog.’ You think your fatigue is unique? It’s not. It’s weakness dressed up as science.
Stop treating your body like a fragile porcelain doll. Exercise. Eat clean. Sleep early. No magic supplements. Just discipline. That’s what real strength looks like.
Jessie Ann Lambrecht
January 9, 2026 AT 04:40Hey, I just want to say-YOU ARE NOT ALONE. I’ve been where you are. I thought I was failing at life because I couldn’t make it through a grocery trip. Then I found pacing. I started with 5 minutes of walking. Then 10. Then I sat down for 10 minutes after. No guilt. No shame.
And CoQ10? I took it for 3 months. My energy didn’t skyrocket, but I went from ‘I can’t hold a cup’ to ‘I can hold a cup and actually taste my coffee.’ That’s huge.
Also, if your doctor doesn’t ask about fatigue, ask THEM. Bring the FACIT-F form. Print it. Hand it to them. You deserve to be seen. Your fatigue is real. Your pain is real. Your life matters-even on the days you’re stuck on the couch.
Ayodeji Williams
January 10, 2026 AT 13:12bro i had the same thing but i tried fasting for 72 hours and now i'm cured lmao
also my cousin's dog had arthritis and he got better after i rubbed lavender oil on his belly so maybe that works too? 🤷♂️
just sayin' maybe you're just not trying hard enough? 😅
also why are you all so dramatic? i mean like... you're not dying? 🥲
Kamlesh Chauhan
January 11, 2026 AT 11:23all this science talk is just noise
you dont need studies to know if you're tired
just get up
my uncle had RA he never took any pills he just drank chai and walked 5 miles every day
you guys are too soft
also why are you using big words like mitochondria
its just tired
why make it complicated
Elen Pihlap
January 11, 2026 AT 17:28i just don’t get why people can’t sleep better
my mom says if you turn off the phone you sleep
i don’t understand why you don’t just do that
you’re all so dramatic
it’s just fatigue
it’s not cancer
why are you making it a big deal
Sai Ganesh
January 12, 2026 AT 02:22Thank you for writing this with such clarity. In India, autoimmune diseases are often dismissed as ‘stress’ or ‘women’s problems.’ I’ve seen too many women told to ‘drink turmeric milk’ and ‘pray more.’
This isn’t spiritual-it’s physiological. The cytokine research? Spot on. The cortisol drop? Real. The mitochondrial dysfunction? Verified in multiple studies.
What we need is not more myths, but more access to testing, specialists, and insurance coverage for CBT-AF and CoQ10. This isn’t a luxury-it’s medical necessity.
And yes, pacing isn’t laziness. It’s strategy. I’ve learned to say ‘no’ to my family’s expectations. My body is my first priority now.
Paul Mason
January 13, 2026 AT 17:09Look, I’ve read all this and I’m just saying-why aren’t you on steroids? I had a mate with RA and he was on prednisone for years. He felt fine. You’re overcomplicating it.
Also, sleep? Everyone says sleep, but do you even have a sleep schedule? I sleep at 10:30 sharp, wake at 6:30, no phone after 9. That’s it.
And CoQ10? It’s a supplement. Not medicine. Don’t waste your cash.
Just get your cortisol checked. If it’s low, ask for hydrocortisone. Done.
Why are you all so confused? It’s basic biology.
Andrew N
January 14, 2026 AT 03:2298% of patients? That’s a cherry-picked stat. The PMC study had a small sample size and selection bias. Also, ‘brain fog’ isn’t a clinical diagnosis-it’s a buzzword.
And pacing? That’s just avoidance behavior. The real solution is exposure therapy. You’re reinforcing disability by rewarding rest.
Also, CoQ10? Placebo effect. Double-blind trials show no significant difference.
People like this article because it validates their helplessness. That’s not science. That’s comfort.
LALITA KUDIYA
January 15, 2026 AT 13:27thank you for this
i have sjogrens and i thought i was going crazy
now i know it’s not me
just my body
❤️
Poppy Newman
January 16, 2026 AT 15:26OMG this is so me 😭
I did the FACIT-F last week and scored 29. My doctor said ‘oh you’re just tired.’
I cried in the parking lot.
CoQ10 is now my best friend 💊
Also pacing = my new religion 🙏
Who else has a timer set for ‘rest mode’? 😅
Anthony Capunong
January 18, 2026 AT 12:56Why are we letting big pharma dictate how we feel? This whole article is a corporate marketing piece. CoQ10? That’s sold in Walmart. Hydrocortisone? Prescription only. Why not just fix your diet? Eat real food. No supplements. No drugs. Just eat like your ancestors did.
Also, why are you all so obsessed with measuring your fatigue? Just live. Stop counting your energy points like it’s a video game.
Vince Nairn
January 19, 2026 AT 16:28so you’re telling me the solution to chronic fatigue is… sitting down
bruh
i’ve got a 9-5 and two kids and i don’t have time to ‘pace’
also who the hell has $200 a month for coq10
you talk like this is a lifestyle blog not a survival guide
we’re not all lucky enough to have a 40-hour work week and a health insurance plan
so thanks for the science but i still gotta pick up my kid from school
and i’m still tired