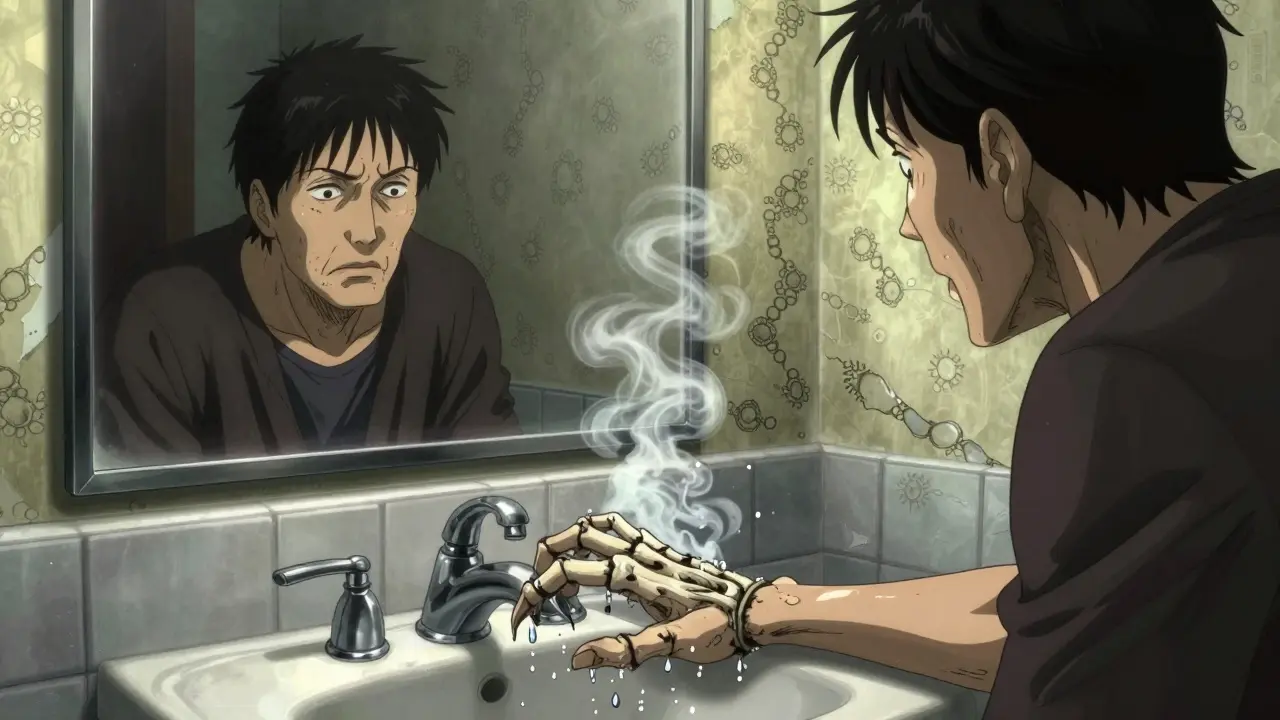
Imagine trying to shake someone’s hand, but your fingers won’t straighten. Or you can’t lay your palm flat on a table. For people with Dupuytren’s contracture, this isn’t rare-it’s everyday life. The condition slowly pulls one or more fingers into the palm, making simple tasks like gripping a coffee cup, typing, or even putting on gloves feel impossible. It’s not painful at first, but over time, it steals function. And while it’s not life-threatening, it can change how you live.
What Exactly Is Dupuytren’s Contracture?
Dupuytren’s contracture is a thickening of the tissue under your palm-the palmar fascia. This tissue normally supports your hand’s structure. But in this condition, it turns into tough, rope-like cords that pull your fingers down. It usually starts with a small, painless lump near the base of your ring or little finger. Over months or years, that lump becomes a cord that tightens and won’t let go.
The name comes from Baron Guillaume Dupuytren, the French surgeon who first described it in 1831. Today, we know it affects 3-6% of people in Western countries. But if you’re over 65 and have Northern European roots-think Scandinavian, British, or Dutch ancestry-your risk jumps to nearly 30%. It’s also more common in men than women, and it often runs in families. If your parent has it, your chance of getting it is about 68%.
Doctors use a simple test to spot it: the table top test. If you can’t lay your hand flat on a table, the cords are already pulling hard enough to interfere. That’s when it’s time to talk about treatment.
How Does It Progress?
This isn’t a sudden problem. It creeps in. Most people go through four stages:
- Stage 1: Small lumps or nodules form in the palm. No pain. No movement loss yet.
- Stage 2: Cords begin to form, stretching from the palm to the fingers. You might notice dimpling or skin puckering.
- Stage 3: Your fingers start bending. Contracture hits 10-30 degrees. You can’t fully open your hand.
- Stage 4: Severe bending-over 45 degrees. Fingers are locked. Daily tasks become hard or impossible.
Progression is unpredictable. For some, it takes 15 years. For others, it races ahead in just a year or two. The American Society for Surgery of the Hand says intervention is usually recommended when the metacarpophalangeal joint (the knuckle) bends more than 30 degrees, or the proximal interphalangeal joint (the middle knuckle) bends over 20 degrees.
Why Does It Happen?
No one knows exactly what triggers Dupuytren’s. But we know a lot about what’s involved.
At the cellular level, abnormal cells called myofibroblasts multiply and produce too much collagen-mainly types I and III. These form the stiff cords that contract with forces stronger than 10 Newtons. That’s like hanging a 2.2-pound weight on your finger. No wonder it won’t straighten.
Genetics play a huge role. Studies have found 11 gene locations linked to the disease, especially on chromosomes 16 and 20. These explain about 25-30% of why some people get it and others don’t. Other factors like smoking, diabetes, alcohol use, and hand trauma may speed things up-but they don’t cause it on their own.
It’s not caused by overuse. You won’t get it from typing too much or lifting weights. It’s not an infection. And no, stretching or massage won’t stop it.
Treatment Options: What Works?
There’s no cure. But there are ways to fix the bend and get your hand back. The right choice depends on how bad the contracture is, your age, your lifestyle, and your tolerance for risk.
Needle Aponeurotomy
This is a quick, minimally invasive procedure. A doctor uses a needle to poke through the skin and cut the cord. No big incision. No hospital stay. You’re walking out the same day.
Success rate? 80-90% for early cases. Recovery is fast-often just a few days. Many people report feeling normal within 48 hours. Guitar players, carpenters, and mechanics love it because they get back to work quickly.
But here’s the catch: recurrence. About 30-50% of people see the cord come back within three years. It’s not a permanent fix, but it’s a great option if you want fast relief without major surgery.
Collagenase Injection (Xiaflex)
This is a two-step process. First, a doctor injects a enzyme called collagenase directly into the cord. The enzyme breaks down the collagen. Then, 24-72 hours later, the doctor manually straightens your finger. It’s like dissolving the rope with chemicals.
Success rate: 65-78% for knuckle bends. It works best on the ring and little fingers. It’s FDA-approved and widely used. But it’s expensive-$3,500 to $5,000 per injection. And you have to follow strict rules: do finger stretches exactly as directed, or success drops from 85% to 65%.
Side effects? Swelling, bruising, and pain are common. Rarely, tendons or nerves get damaged. But complication rates are lower than surgery-only 5.2% compared to 18.7% for open procedures.
Open Fasciectomy
This is the traditional surgery. The surgeon cuts open the palm and removes the entire abnormal tissue. It’s the most thorough option. Success rate? 90-95% correction. Recurrence? Only 20-30% after five years.
But it’s not simple. Recovery takes 6-12 weeks. You’ll need physical therapy. There’s a 3-5% risk of nerve damage. And if you have severe disease or had surgery before, the scar tissue can make it harder next time.
There’s also a variation called dermofasciectomy, where the skin over the cord is removed and replaced with a skin graft. This cuts recurrence down to 10-15%, but recovery stretches to 3-6 months. It’s used for aggressive cases or people who’ve had multiple recurrences.
What Doesn’t Work
Many people try things that sound logical-but don’t help.
Corticosteroid injections: They might ease pain in early nodules, but they don’t stop cords from forming. Studies show only a 30% response rate, and they can thin the skin over time.
Stretching gloves or splints: These are marketed heavily online. But a 2023 survey found 28% of users reported skin breakdown and no real improvement. They’re not recommended by hand specialists as a primary treatment.
Herbal remedies, acupuncture, or ultrasound therapy: No solid evidence supports them. Don’t waste money.
Cost and Value: What’s Worth It?
Treatment costs vary wildly:
| Treatment | Average Cost | Success Rate | Recurrence Rate (3-5 years) | Recovery Time |
|---|---|---|---|---|
| Needle Aponeurotomy | $1,500-$3,000 | 80-90% | 30-50% | Days to 1 week |
| Collagenase (Xiaflex) | $3,500-$5,000 | 65-78% | 20-35% | 1-2 weeks |
| Open Fasciectomy | $8,000-$15,000 | 90-95% | 20-30% | 6-12 weeks |
| Dermofasciectomy | $10,000-$18,000 | 90-95% | 10-15% | 3-6 months |
Cost per degree of correction? Needle aponeurotomy wins at $75 per degree. Collagenase is $120. Surgery is more expensive upfront but lasts longer. If you’re young and active, you might need multiple treatments over your lifetime. That’s why some surgeons recommend waiting until contracture hits 30 degrees before acting.
Real People, Real Stories
One Reddit user, ‘PalmProblem89,’ couldn’t shake hands or put his hands in his pockets. After Xiaflex, he got 70% improvement-but the finger straightening hurt like hell. Another, ‘GuitarGuy42,’ had needle aponeurotomy and was playing guitar again in two days.
A 2023 survey of over 1,200 patients found:
- 89% had trouble gripping things
- 76% struggled with washing or dressing
- 68% said it affected their job
- Manual laborers were 3.2 times more likely to lose work time than office workers
It’s not just about function-it’s about dignity. People avoid social situations. They feel embarrassed. That’s why early intervention matters, even if the bend seems small.
What Should You Do?
If you notice a lump or can’t flatten your palm:
- See a hand specialist-not a general doctor. Look for an orthopedic surgeon who focuses on hands.
- Get a goniometer reading. That’s the tool that measures how many degrees your finger is bent. Apps like ‘Hand Meter’ are surprisingly accurate.
- Don’t rush into surgery. If your contracture is under 30 degrees, many experts recommend watchful waiting. About 40% of people never progress to functional loss.
- If you’re over 50, have a family history, or your job relies on your hands, consider treatment sooner.
- Ask about recurrence rates and recovery time. This isn’t a one-size-fits-all fix.
And if you’re worried about genetics? Talk to your family. If your parent or sibling has it, you should check your hands yearly. Early detection means simpler, cheaper treatment.
What’s Coming Next?
The future of Dupuytren’s treatment is exciting. Gene therapy targeting the TGF-β1 protein is already in early trials. One study showed a 40% reduction in cord thickness after six months.
There’s also a new device called the Fasciotome, cleared by the FDA in March 2023. It uses ultrasound guidance to cut cords through a tiny needle-cutting procedure time from 30 minutes to just 12.
And researchers are testing stem cell therapy from fat tissue. Early results show a 55% drop in recurrence after two years. That could be a game-changer.
For now, though, the tools we have work well. The key is knowing when to act-and choosing the right one for your life.
Can Dupuytren’s contracture go away on its own?
No. Dupuytren’s contracture doesn’t reverse itself. The cords don’t dissolve or loosen over time. Without treatment, the bend will either stay the same or get worse. Some people live with mild cases for years without major issues, but the tissue changes are permanent. The goal of treatment isn’t to cure-it’s to restore function.
Is Dupuytren’s contracture painful?
Usually not. The nodules might be tender at first, especially when they’re new. But once the cords form, most people feel no pain-just stiffness and restriction. If you’re experiencing sharp pain, burning, or numbness, it could be nerve involvement or another condition like carpal tunnel. See a specialist to rule that out.
Can I prevent Dupuytren’s contracture?
Not really. Since genetics play such a strong role, you can’t prevent it if you’re predisposed. Smoking and heavy alcohol use may speed it up, so quitting helps. But stretching, massage, or supplements won’t stop it. The best prevention is early detection. Check your hands every few months. If you see a lump or can’t flatten your palm, get it checked.
Will I need more than one treatment?
Very likely. Recurrence is common. Needle aponeurotomy has a 30-50% chance of the cord coming back in three years. Even surgery has a 20-30% recurrence rate. That doesn’t mean failure-it means the condition is chronic. Many people get a second needle procedure, or even a third. The goal is to maintain function over time, not to fix it once and forget it.
Does insurance cover Dupuytren’s treatments?
Yes, most major insurance plans cover needle aponeurotomy, collagenase injections, and surgery when they’re medically necessary. But coverage varies. Collagenase is expensive, so some insurers require you to try physical therapy or splinting first-even though those aren’t proven effective. Always check with your provider and ask for pre-authorization. Out-of-pocket costs can be high if you’re uninsured.
Can Dupuytren’s affect both hands?
Yes, about half of all patients have it in both hands. But it’s rarely symmetrical. One hand is usually worse by 15-25 degrees. That’s why doctors always check both hands-even if only one feels problematic. Treating the worse hand first often gives the biggest improvement in daily function.
How do I know if I need surgery?
You don’t need surgery just because you have a lump. The decision is based on function, not appearance. If you can’t lay your hand flat on a table, or if your finger bend is over 30 degrees at the knuckle, it’s time to consider treatment. If your job, hobbies, or personal care are affected, surgery might be worth it. If you’re just noticing a bump and your hand still works fine, wait and monitor. Many people never need surgery.


Angela Goree
January 1, 2026 AT 17:16Brittany Wallace
January 3, 2026 AT 06:18Liam Tanner
January 4, 2026 AT 23:24Palesa Makuru
January 6, 2026 AT 06:33Hank Pannell
January 6, 2026 AT 20:02Wren Hamley
January 7, 2026 AT 15:50Sarah Little
January 8, 2026 AT 18:29innocent massawe
January 9, 2026 AT 04:07