Depression isn’t just feeling sad. It’s waking up exhausted, skipping meals because food tastes like ash, and staring at the ceiling for hours because getting out of bed feels impossible. For 280 million people worldwide, this isn’t a phase-it’s a daily reality. And the good news? It doesn’t have to stay that way. Modern depression management isn’t about one magic fix. It’s about combining the right medications, proven therapy, and real-life lifestyle changes-tailored to your body, your mind, and your life.
Medications: Not a Quick Fix, But a Tool
When people think of depression treatment, they often jump straight to pills. And yes, antidepressants work-but not for everyone, and not the same way for everyone. The first-line choices today are second-generation antidepressants, especially SSRIs like sertraline, citalopram, and fluoxetine. These aren’t the old-school drugs from the 1980s. They’re safer, better tolerated, and backed by decades of data.Why sertraline? It’s often the go-to because it’s affordable, effective, and doesn’t knock people out or make them gain weight like some older meds. But here’s the catch: side effects are real. About 30 to 50% of people on SSRIs experience sexual dysfunction. That’s not a footnote-it’s a dealbreaker for some. SNRIs like venlafaxine can raise blood pressure in 10 to 15% of users. Bupropion? It’s less likely to cause sexual side effects, but it carries a small seizure risk-about 1 in 250 people at standard doses.
For mild depression, guidelines like NICE’s 2022 update say: skip the meds unless you really want them. For moderate to severe cases, medication is a solid option. But here’s what most people don’t know: antidepressants take 4 to 8 weeks to show real effects. If you stop after two weeks because you feel nothing, you’re not failing-you’re just not giving it time.
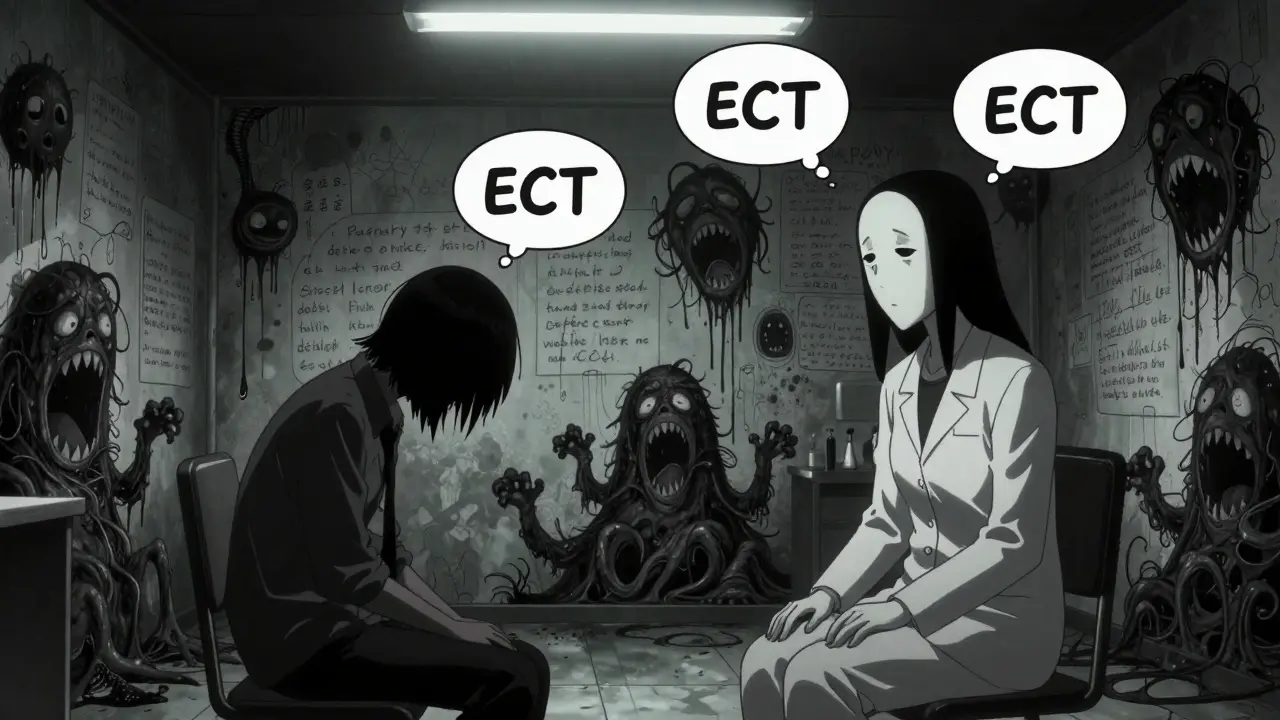
If two different antidepressants don’t help after 8 to 12 weeks each, you’re looking at treatment-resistant depression. That’s not the end. Augmentation strategies like adding low-dose quetiapine or lithium can push response rates from 20% to over 50%. Electroconvulsive therapy (ECT) still has the highest success rate-70 to 90% remission in severe cases-even if memory issues are a concern for some. And yes, it’s still used today, even in Australia, for people who haven’t responded to anything else.
Therapy: Talking Is Medicine
Therapy isn’t just for people who "can’t handle their emotions." It’s a structured, evidence-based treatment. Cognitive Behavioral Therapy (CBT) is the gold standard. In 8 to 28 weekly sessions, you learn to spot thought patterns that feed depression-like "I’m worthless because I didn’t reply to a text"-and replace them with something more realistic. Studies show CBT gives a 50 to 60% response rate in mild to moderate depression. That’s as good as medication.Interpersonal Therapy (IPT) works differently. It focuses on relationships-grief, conflict, isolation-that might be fueling your depression. If you’ve lost someone, been abandoned, or feel trapped in a toxic relationship, IPT helps untangle that. It’s not fluff. A 2016 meta-analysis showed 55% of people improved with IPT, compared to 45% in control groups.
For people who’ve had depression before, Mindfulness-Based Cognitive Therapy (MBCT) is a game-changer. It’s an 8-week group program that teaches you to notice negative thoughts without getting swept away by them. The PREVENT trial found it cut relapse risk by 31% over a year. That’s not minor. It’s life-changing for someone who’s been through this three or four times.
And if your depression is tied to your relationship? Behavioral couples therapy can help. One study showed 40 to 50% symptom improvement when both partners worked on communication-better than individual therapy alone. Therapy isn’t just about you. Sometimes, it’s about how you connect with others.
Lifestyle Changes: The Forgotten Pill
We talk about pills and therapy, but what about the things you do every day? Movement. Sleep. Food. These aren’t "nice-to-haves." They’re treatment.Exercise isn’t about getting ripped. It’s about moving enough to raise your heart rate. Three to five sessions a week of brisk walking, cycling, or swimming-30 to 45 minutes each-can match the effects of antidepressants for mild depression. A 2020 meta-analysis found it had a standardized effect size of -0.68. That’s clinically meaningful. You don’t need a gym. You just need to get up and move.
Sleep is even more critical. About 75% of people with depression struggle with insomnia. Fixing sleep doesn’t just help you feel rested-it reduces depression severity by 30 to 40%. The protocol? Go to bed and wake up at the same time, even on weekends. Stay in bed only when you’re sleepy. No screens an hour before bed. Keep your bedroom cool and dark. Simple. Hard to do. Life-changing.
Diet matters more than you think. The SMILES trial gave people with depression a 12-week Mediterranean diet: lots of vegetables, fruits, whole grains, fish, olive oil, and nuts. No processed food, no sugar. After three months, 32% went into remission. Only 8% did in the control group, which got social support instead. That’s not a diet. That’s a treatment.
Stress reduction techniques like daily 10-minute mindfulness, yoga twice a week, or tai chi can lower depression symptoms with moderate effect sizes. You don’t need to meditate for an hour. Ten minutes while sipping tea in the morning? That’s enough.
What Works Based on How Bad It Is
Depression isn’t one-size-fits-all. Treatment should match severity.- Mild (PHQ-9: 5-9): Skip meds unless you ask for them. Try structured exercise, guided self-help apps, or weekly check-ins with a clinician.
- Moderate (PHQ-9: 10-14): Choose between CBT or an SSRI. Both work. Combine them if you’re struggling to function-work, relationships, daily tasks.
- Severe (PHQ-9: 15+): Start with both medication and therapy. Alone, either one gives you a 40-50% chance of improvement. Together? 60-70%. That’s the difference between surviving and starting to live.
- Chronic (2+ years): CBASP (Cognitive Behavioral Analysis System of Psychotherapy) is designed for this. It’s complex, but studies show 48% response with CBASP plus meds, compared to 28% with meds alone.
- Psychotic depression: This is a medical emergency. Antidepressants plus antipsychotics-or ECT-are needed. ECT works in 70-80% of cases.
There’s no shame in needing more than one thing. Most people who get better use a mix.

Barriers and What’s New
Here’s the hard truth: only 35.6% of adults with depression in the U.S. get any treatment. Mental health workers are in short supply. Waitlists are long. That’s why digital tools are rising. FDA-cleared apps like reSET show a 47% response rate in trials. They’re not replacements, but they help when therapy isn’t available.Telehealth has exploded. In 2019, only 18% of providers offered video visits. By 2022, it was 68%. In Melbourne, you can now see a psychiatrist from your couch. That’s progress.
New treatments are on the horizon. Psilocybin-yes, from magic mushrooms-showed a 71% response rate in a 2021 trial. It’s not legal yet, but it’s coming. Digital phenotyping uses your phone’s sensors to track your voice, steps, and texting patterns to predict a depressive episode 7 days ahead. Accuracy? 82%.
And the biggest shift? Personalization. We’re done with "take this pill and call me in six weeks." Now, we ask: What’s your sleep like? Do you have chronic pain? Are you isolated? Are you a parent? A caregiver? A veteran? Your treatment should fit your life-not the other way around.
Final Thought: It’s Not About Willpower
Depression isn’t weakness. It’s biology. It’s brain chemistry. It’s stress, trauma, and genetics tangled together. You don’t need to "snap out of it." You need the right combination of tools.Start small. One walk. One therapy session. One night of no screens. One meal with vegetables. You don’t have to fix everything at once. Progress isn’t linear. Some days, just getting out of bed is the win.
And if you’re reading this because you’re struggling-know this: you’re not alone. Millions are walking this path. And with the right mix of medication, therapy, and lifestyle, you can walk out of it too.
How long does it take for antidepressants to work?
Most antidepressants take 4 to 8 weeks to show noticeable effects. Some people feel slight improvements in energy or sleep after 2 weeks, but full benefits usually take longer. Stopping early because you don’t feel better right away is the most common reason treatment fails. Stick with it for at least 6 to 8 weeks at the right dose before deciding if it’s working.
Can therapy replace medication for depression?
For mild to moderate depression, yes-therapy like CBT or IPT can be just as effective as medication. For severe depression, combining both gives the best results. Some people prefer therapy to avoid side effects. Others need medication to get well enough to engage in therapy. There’s no single right answer-it depends on your symptoms, history, and preferences.
Is exercise really as effective as antidepressants?
For mild depression, yes. A 2020 meta-analysis found that 3 to 5 sessions per week of moderate exercise (like brisk walking) had an effect size comparable to SSRIs. It doesn’t mean exercise works for everyone, but it’s one of the few treatments with zero side effects and added benefits for heart health, sleep, and self-esteem. It’s not a cure, but it’s a powerful tool.
What if I’ve tried everything and still feel depressed?
You’re not alone. About 30% of people have treatment-resistant depression. The next steps include switching medications, adding an augmenting agent like lithium or quetiapine, or trying advanced treatments like rTMS (repetitive transcranial magnetic stimulation), which has a 50-55% response rate. ECT remains the most effective option for severe cases. Don’t give up-there are still options, and new ones are emerging all the time.
Can diet really change how I feel?
The SMILES trial proved it. People who followed a Mediterranean diet for 12 weeks had a 32% remission rate-nearly four times higher than those who got social support alone. Food affects brain inflammation, gut bacteria, and neurotransmitter production. You don’t need to be perfect, but cutting out processed sugar and junk food while adding more vegetables, fish, nuts, and whole grains can make a real difference.
Are digital apps for depression actually helpful?
Yes, but only certain ones. FDA-cleared digital therapeutics like reSET have been tested in clinical trials and show a 47% response rate. They’re not substitutes for therapy or medication, but they’re useful for tracking mood, practicing CBT skills, or staying connected when in-person care isn’t available. Avoid apps that promise instant fixes or sell unproven supplements.
How do I know if I need medication?
If your depression is keeping you from working, caring for yourself, or connecting with loved ones-if you’ve lost interest in everything for more than two weeks-it’s time to talk to a doctor. Medication isn’t a sign of failure. It’s a tool to help your brain heal. Your doctor will consider your symptoms, past treatments, side effect risks, and preferences before recommending anything.


Shelby Price
February 3, 2026 AT 09:38also, the sexual side effects? yeah. that part sucked. but i'd take it over crying in the shower every morning.
Antwonette Robinson
February 5, 2026 AT 04:47Mandy Vodak-Marotta
February 5, 2026 AT 07:32Zachary French
February 5, 2026 AT 08:20also, why is everyone ignoring the fact that 70% of antidepressant trials are funded by drug companies? this is just a rebranded supplement ad with a fancy study name.
Daz Leonheart
February 6, 2026 AT 11:41Kunal Kaushik
February 8, 2026 AT 09:10Lorena Druetta
February 9, 2026 AT 09:18Sherman Lee
February 11, 2026 AT 04:08Nathan King
February 11, 2026 AT 12:29Samuel Bradway
February 13, 2026 AT 01:49Keith Harris
February 13, 2026 AT 21:13Jesse Naidoo
February 14, 2026 AT 13:40