For people with cutaneous lupus, a single day at the park, a walk to the car, or even sitting near a window can trigger a painful, visible flare. It’s not just a sunburn-it’s an autoimmune reaction, often delayed by days, that turns skin red, scaly, or scarred. And here’s the hard truth: photosensitivity isn’t just a symptom. It’s the main driver of skin damage in up to 75% of lupus patients.
Why Sunlight Turns Into a Skin Flare
It’s not that sunlight causes lupus. But if you already have it, UV rays act like a match to dry tinder. Both UVA and UVB light penetrate the skin and trigger a chain reaction in immune cells. Keratinocytes-the skin’s outer layer cells-start dying off faster than normal. In lupus patients, this happens 2.3 times more than in people without the disease. When those cells die, they spill out proteins that the immune system doesn’t recognize. It sees them as invaders and attacks.This isn’t just inflammation. It’s a full-blown immune signal. UV exposure causes skin cells to pump out interferon-kappa (IFN-κ), a cytokine that’s already overactive in lupus. Levels can spike by 400-600%. That tells other immune cells to rush in. Chemokines like CCL5 and CCL8 surge by 300%, pulling in more inflammatory cells. The result? A rash that shows up 24 to 72 hours later and can last for weeks.
And it’s not just the sun. Fluorescent lights, especially CFLs, emit enough UV to trigger reactions. One patient on Reddit described developing a full butterfly rash after 15 minutes by a window. That’s UVA passing through glass-something most people don’t realize can still cause damage.
The Three Faces of Lupus Skin Rashes
Not all cutaneous lupus rashes look the same. The type you get depends on your immune profile and how your skin reacts to UV exposure.- Acute cutaneous lupus (ACLE) shows up as the classic butterfly rash across the cheeks and nose. It’s red, flat, and often burns. About 85% of ACLE cases are triggered by sunlight. This rash doesn’t scar, but it’s a red flag-up to 60% of people with ACLE will later develop systemic lupus.
- Subacute cutaneous lupus (SCLE) appears as red, scaly patches that look like ringworm or psoriasis. They’re often on the arms, shoulders, or neck. About 92% of SCLE patients have photosensitivity. These lesions don’t scar, but they’re stubborn and often misdiagnosed as eczema or fungal infections.
- Chronic cutaneous lupus (CCLE), or discoid lupus, causes thick, scaly, disk-shaped lesions, usually on the scalp, ears, or face. These scars permanently damage skin and hair follicles. Sun exposure doesn’t always cause new ones, but it makes existing ones worse. About 76% of discoid patients report flare-ups after UV exposure.
Here’s the tricky part: nearly half of people diagnosed with photosensitivity actually have something else-like polymorphous light eruption (PMLE). The difference? PMLE fades within days and doesn’t cause scarring. True lupus photosensitivity lasts longer than three weeks in 89% of cases. That’s why a skin biopsy is often needed to confirm.

What Treatments Actually Help the Skin
There’s no cure for cutaneous lupus, but you can stop flares before they start. The most effective tool isn’t a pill-it’s protection.Sunscreen isn’t optional-it’s medical equipment. The Lupus Foundation of America recommends SPF 50+ with zinc oxide or titanium dioxide. These are physical blockers, not chemical filters. They sit on top of the skin and reflect UV rays. Chemical sunscreens absorb UV, which can sometimes irritate sensitive lupus skin. Reapply every two hours-even if you’re indoors near a window. Studies show consistent use cuts flares by 87%.
UPF 50+ clothing blocks 98% of UV radiation. Regular cotton t-shirts only block about 5%. Specialized sun-protective clothing from brands like Coolibar or Solumbra is worth the investment. Wear wide-brimmed hats, long sleeves, and UV-blocking gloves-even in spring and fall.
Window film is one of the most underused tools. Standard glass blocks UVB but lets through 75% of UVA. Installing UV-blocking film on home and car windows reduces UVA transmission by 99.9%. Many patients report dramatic improvement after installing it.
Lighting matters. Replace fluorescent bulbs with LED. LEDs emit 92% less UV. If you work under fluorescent lights, ask your employer to switch them out. Companies like Microsoft and Johnson & Johnson have already done this in most North American offices.
Eye protection is often ignored. Up to 70% of lupus patients have photophobia. FL-41 tinted lenses-those rose-colored glasses-are clinically proven to reduce light sensitivity by 68%. They’re not fashion accessories. They’re therapy.
When Sunscreen Isn’t Enough: Medications for the Skin
If you’re doing everything right and still getting flares, it’s time to look at targeted treatments.Topical calcineurin inhibitors like tacrolimus (Protopic) and pimecrolimus (Elidel) are steroid-free options that calm inflammation without thinning the skin. They’re especially helpful for sensitive areas like the eyelids or lips.
Antimalarials like hydroxychloroquine (Plaquenil) are the first-line oral treatment. They don’t just treat joint pain-they stabilize the immune system’s response to UV. Studies show they reduce skin flares by up to 50%. They take weeks to work, but they’re the backbone of long-term control.
Anifrolumab, approved by the FDA in 2021, is a newer option. It blocks the interferon receptor-the very pathway that UV light overactivates. In clinical trials, patients with photosensitivity saw 34% greater improvement in skin lesions compared to placebo. It’s not for everyone, but for those with severe, sun-triggered rashes, it’s a game-changer.
JAK inhibitors like baricitinib are in phase II trials and show promise. By blocking interferon signaling, they reduce photosensitivity reactions by 55% in early studies. They’re not yet approved for skin-only lupus, but many dermatologists are prescribing them off-label for stubborn cases.
What No One Tells You
Most patients say their biggest struggle isn’t the rash-it’s being dismissed. Over half of people surveyed by the Lupus Foundation of America had their photosensitivity ignored by their primary care doctor. They were told to “just use sunscreen” or “it’s probably just eczema.”But this isn’t just about comfort. Every flare increases the risk of organ damage. Skin flares are often the first sign that the immune system is getting out of control. Ignoring them can lead to kidney, lung, or heart involvement down the line.
Also, not all sunscreens are equal. Avoid sprays-they’re hard to apply evenly. Skip products with fragrances, alcohol, or parabens. Look for “hypoallergenic” and “non-comedogenic.” And never assume a high SPF means all-day protection. Reapply. Always.
What’s Next: Smart Protection
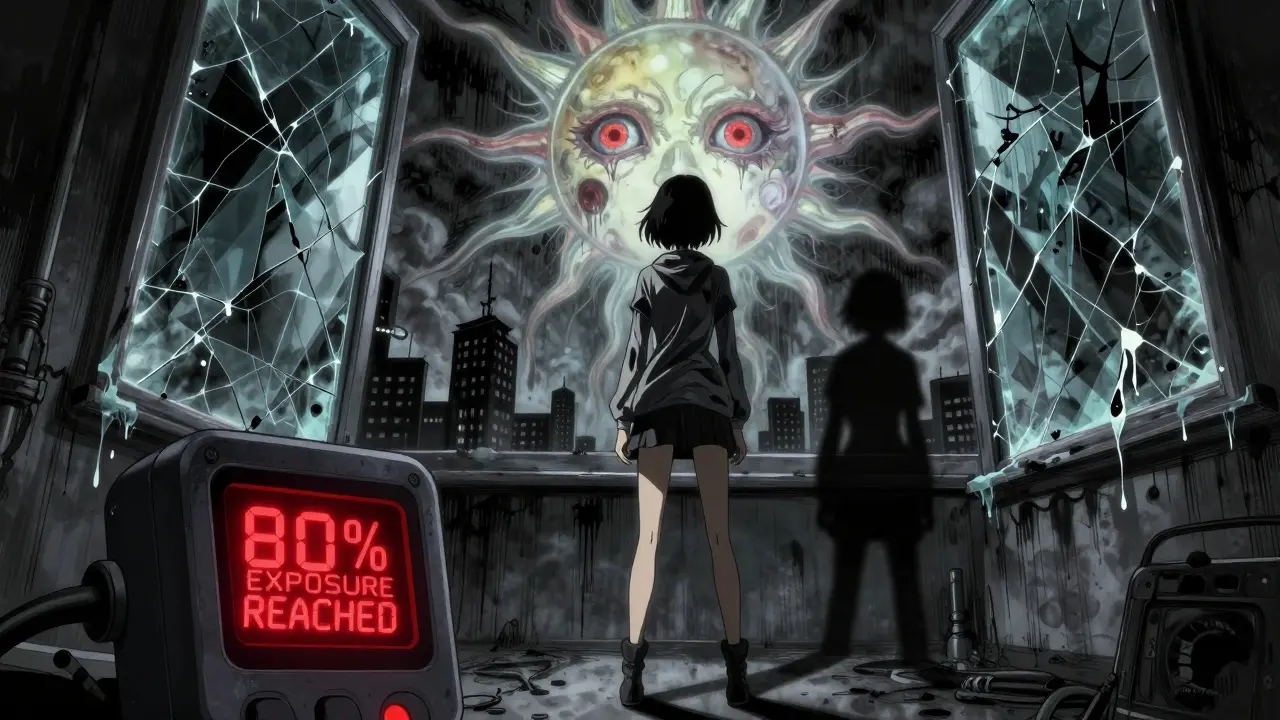
The future of lupus skin care is getting smarter. Three wearable UV monitors are now in clinical testing. They track your daily exposure and send alerts when you’re at risk. One device, tested on 200 lupus patients, predicted flare risk with 92% accuracy. Imagine getting a text: “You’ve hit 80% of your daily UV limit. Head indoors.”Workplaces are catching on too. Since 2020, companies have increased UV accommodations by 42%. More offices are installing window film, switching to LED lighting, and allowing flexible hours to avoid midday sun.
The message is clear: you can’t out-run lupus. But you can out-smart it. With the right tools, most skin flares are preventable. And preventing flares isn’t just about looking better-it’s about keeping your whole body healthy.
Can you get lupus skin flares from indoor lighting?
Yes. Compact fluorescent lights (CFLs) emit UV radiation, enough to trigger reactions in up to 74% of lupus patients who report light sensitivity. LED bulbs emit 92% less UV and are the recommended replacement. Even sitting near a window indoors can cause flares because glass blocks UVB but not UVA.
Is sunscreen enough to prevent lupus skin flares?
Sunscreen is necessary but not always sufficient. For best results, combine it with UPF 50+ clothing, UV-blocking window film, and avoiding midday sun. Studies show that people who use sunscreen alone still have flares 45% of the time. Those who use a full photoprotection plan reduce flares by up to 70%.
Why does my rash appear days after sun exposure?
Lupus photosensitivity reactions are delayed because the immune response takes time. UV light triggers cell death and interferon release, which then recruits inflammatory cells to the skin. Symptoms typically appear 24-72 hours later. If the rash lasts more than 3 weeks, it’s likely true lupus-not just a sun allergy.
Do I need a skin biopsy if I have a sun-triggered rash?
Yes, if the rash is persistent or recurring. About 49% of people diagnosed with photosensitivity actually have polymorphous light eruption (PMLE), not lupus. A biopsy can distinguish between the two. Lupus rashes show specific immune cell patterns and interface dermatitis that PMLE doesn’t.
Can I still go outside if I have cutaneous lupus?
Absolutely-but you need a plan. Avoid direct sun between 10 a.m. and 4 p.m. Wear UPF clothing, a wide-brimmed hat, and UV-blocking sunglasses. Apply zinc oxide sunscreen every two hours. Many patients live full, active lives by using these tools consistently. It’s not about avoiding the sun-it’s about managing exposure.
Are there new treatments on the horizon for lupus skin rashes?
Yes. Anifrolumab, approved in 2021, targets the interferon pathway directly triggered by UV light and reduces skin lesions significantly. JAK inhibitors like baricitinib are in late-stage trials and show 55% reduction in photosensitivity reactions. Wearable UV monitors that predict flare risk are also entering clinical use, helping patients avoid exposure before it starts.


Brian Furnell
December 21, 2025 AT 21:12Okay, so let me get this straight: UV-induced keratinocyte apoptosis triggers IFN-κ upregulation, which then cascades into CCL5/CCL8 chemokine surges, recruiting inflammatory infiltrates? That’s not just photosensitivity-that’s a targeted immune detonation. And the fact that UVA penetrates glass? That’s why indoor exposure is non-negotiable. I’ve seen patients with discoid lesions worsen after sitting by a south-facing window for 20 minutes. No one tells you this. No one.
Physical blockers like zinc oxide aren’t just ‘better’-they’re non-negotiable. Chemical filters? They’re metabolic stressors for lupus skin. I’ve seen reactions to avobenzone. It’s not paranoia-it’s pathophysiology.
Siobhan K.
December 22, 2025 AT 15:21So let me understand-you’re telling me that my fluorescent-lit cubicle is basically a UV bomb, and my sunscreen is useless if I’m not wearing UPF 50+ clothing and window film? And the fact that my doctor told me to ‘just stay out of the sun’ is the medical equivalent of telling a diabetic to ‘just eat less sugar’?
Thanks for validating my five-year battle with misdiagnosed SCLE. I’m not lazy. I’m not overreacting. I’m just living in a world that refuses to see invisible autoimmune warfare.
Dan Adkins
December 22, 2025 AT 17:23It is imperative to note that the aforementioned pathophysiological mechanisms are not universally applicable across all ethnic subpopulations. In particular, the prevalence of photosensitivity in African-derived populations is significantly lower than in Caucasoid cohorts, as documented in the Journal of Cutaneous Immunology and Rheumatology, Volume 17, Issue 3, 2022.
Furthermore, the recommendation to replace fluorescent lighting with LED technology is a Western-centric solution that does not account for infrastructural limitations in developing nations. The cost-benefit analysis of UV-blocking window film is economically untenable for the majority of the global population. One must consider socioeconomic determinants of health before prescribing photoprotection as a universal standard.
Grace Rehman
December 23, 2025 AT 08:09So we’re supposed to believe that the same sunlight that gives us vitamin D and serotonin is secretly plotting to turn our skin into a battlefield? And the cure is to live like a mole in a lead-lined bunker?
Maybe the real problem isn’t lupus. Maybe it’s that we’ve forgotten how to live with nature instead of trying to banish it with SPF 50 and LED bulbs. I’m not saying skip protection-but maybe stop treating your skin like a lab sample and start treating it like a living thing.
Also FL-41 glasses? Those look like something a 90s goth band wore on tour. I’m not wearing them. No amount of clinical trials will make me look like I’m auditioning for a vampire movie.
Adrian Thompson
December 24, 2025 AT 22:48They don’t want you to know this but the WHO and Big Pharma are hiding the truth-UV isn’t the enemy. It’s the vaccines. The mRNA shots alter your skin’s immune memory. That’s why you’re suddenly reacting to sunlight after getting your booster. The government knows. That’s why they’re pushing window film and LED lights-so you can’t see the sun and question the agenda.
Also, fluorides in toothpaste and water are what’s really triggering this. It’s not the CFLs. It’s the sodium fluoride poisoning. They don’t want you to know that. Google ‘lupus fluoride correlation’ and you’ll find the suppressed studies.
Jackie Be
December 25, 2025 AT 01:58OMG YES I’ve been living this. I thought I was just bad at sunscreen until I got a rash after sitting next to my window while working from home. I thought it was my new soap. Then my dermatologist said ‘oh that’s SCLE’ and I cried for three hours.
I bought the Coolibar hat and the FL-41 glasses and I look like a space alien but I haven’t had a flare in 6 months. I’m not even joking. I wear the glasses to the grocery store. People stare. I don’t care. I’m alive.
Also I just found out my car windows don’t block UVA. I’m getting film installed tomorrow. My car is now a fortress.
John Hay
December 27, 2025 AT 01:51That’s a solid breakdown. I’ve been on hydroxychloroquine for 3 years and it’s the only thing keeping me from being housebound. But honestly, the biggest win was the window film. I didn’t realize how much UVA was coming through my living room windows until I installed it. My rash went from weekly to once every 4 months.
Also agree on the sunscreen thing. I used to use chemical ones because they didn’t leave a white cast. Then my face looked like a lava lamp. Switched to zinc oxide and no more burning. Simple. Effective. No drama.
Jon Paramore
December 28, 2025 AT 19:41Interferon-kappa is the linchpin. UV → keratinocyte stress → DAMPs → TLR activation → IFN-κ → JAK/STAT → chemokine cascade. That’s the core pathway. Anifrolumab blocks IFNAR1, so it directly interrupts this. JAK inhibitors like baricitinib hit downstream. That’s why they’re showing 55% reduction in photosensitivity-targeting the same axis.
Also, UPF 50+ clothing isn’t marketing. It’s physics. Cotton at 5% UPF? That’s worse than no protection. You need woven fibers with titanium dioxide or zinc oxide integrated into the yarn. Not just ‘sun-protective’ labels-actual certified UPF 50+.
Teya Derksen Friesen
December 30, 2025 AT 12:29Thank you for writing this with such precision. I’ve spent years being told I’m ‘too sensitive’ or ‘just anxious.’ This isn’t anxiety. This is biology. I wear my UPF gloves while gardening. I use LED bulbs in every lamp. I’ve installed UV film on my home windows. It’s expensive. It’s inconvenient. But it’s the difference between being able to hold my child and being in bed for weeks.
I’m not asking for sympathy. I’m asking for recognition. This isn’t a lifestyle choice. It’s a medical necessity.
Cara C
December 31, 2025 AT 15:37Just wanted to say thank you. I’ve been living with discoid lupus for 12 years. I thought I was the only one who got flares from office lighting. I’ve been using the FL-41 glasses for a year now. I didn’t think they’d work. But they did. My eyes don’t ache anymore. My skin flares are less severe. I’m not cured. But I’m not defeated anymore either.
You’re not alone.