A cerebral aneurysm isn’t something you hear about until it’s too late. Most people never know they have one-until it bursts. About cerebral aneurysm affects 1 in 30 adults globally, and while many never cause problems, a rupture is devastating. Around 10 in every 100,000 people experience a brain aneurysm rupture each year. Half of those don’t make it past the first day. The good news? If caught early, you can stop it before it happens.
What Makes a Brain Aneurysm Likely to Burst?
Not all aneurysms are created equal. Size matters-but not the whole story. An aneurysm larger than 7 mm has over three times the risk of bursting compared to smaller ones. But even a 4 mm aneurysm in the right spot can be dangerous. The anterior communicating artery, a small vessel near the front of the brain, is one of the most common rupture sites-even when the aneurysm is tiny. That’s why location is just as important as size.
Shape plays a huge role too. Aneurysms with irregular bulges, daughter sacs, or lobes are far more likely to rupture than smooth, round ones. Think of it like a balloon: a perfectly round one holds pressure better. A lopsided one? It’s already under stress. Studies show irregular shapes carry nearly 3 times the rupture risk.
Then there’s blood flow. The way blood pushes against the weakened wall creates invisible forces. Low, swirling blood flow-called oscillatory shear stress-is found in 83% of ruptured aneurysms. It’s not just about how big the bulge is; it’s about how the blood moves around it. This is why some aneurysms grow slowly and never burst, while others explode without warning.
Who’s at Highest Risk?
You can’t change your age or gender, but knowing your risks helps. If you’re over 65, your rupture risk is nearly three times higher than someone in their 40s. Women are more likely than men to develop aneurysms-and more likely to have them rupture. Family history? If two or more close relatives had one, your risk jumps fourfold.
But the biggest modifiable risks? Smoking and high blood pressure. Smokers are more than three times as likely to rupture an aneurysm. And it’s not just smoking-it’s how much. People who smoke 10 or more cigarettes a day raise their risk by almost 50%. Quitting cuts that risk by over half within two years.
Hypertension is even more dangerous. A systolic blood pressure above 140 mmHg triples your rupture risk. That’s why controlling blood pressure isn’t just about heart health-it’s a brain-saving habit. Heavy drinking also adds risk: more than 14 drinks a week bumps up the chance by over 30%.
And if you’ve already had one rupture? Your chance of another is more than five times higher. Multiple aneurysms? That’s a 3.8 times greater risk. These aren’t just numbers-they’re red flags.
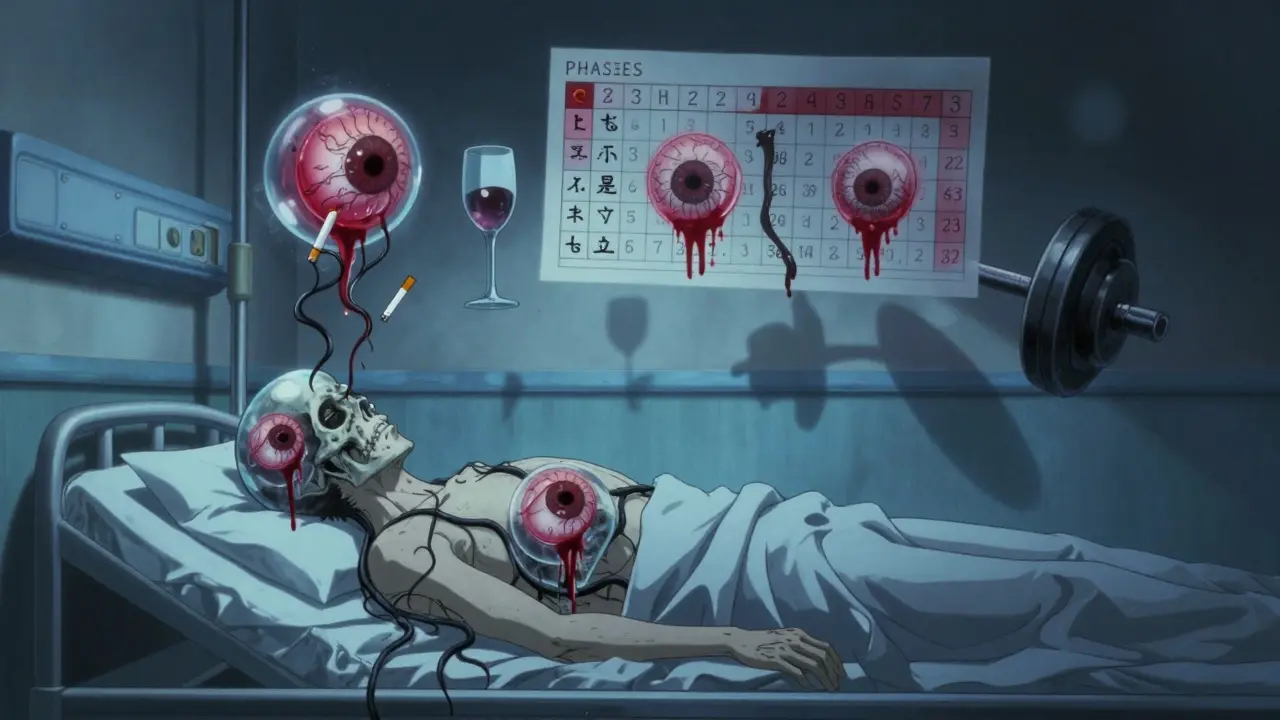
The PHASES Score: Your Personal Rupture Risk Calculator
Doctors don’t guess. They use tools. The PHASES score is the gold standard for predicting rupture risk over five years. It adds up six factors: where you live (population risk), whether you have high blood pressure, your age, the size of the aneurysm, if you’ve had a previous rupture, and its location.
The score runs from 0 to 10. A score of 0-3? Your five-year rupture risk is about 3%. A score of 9-10? That’s a 45% chance. Most doctors use this to decide: treat or watch.
If your score is 6 or higher, treatment is usually recommended. Below 6? Monitoring with yearly MRA scans is often enough. This isn’t one-size-fits-all. A 5 mm aneurysm in the back of the brain might be riskier than a 7 mm one in the front. PHASES accounts for that.
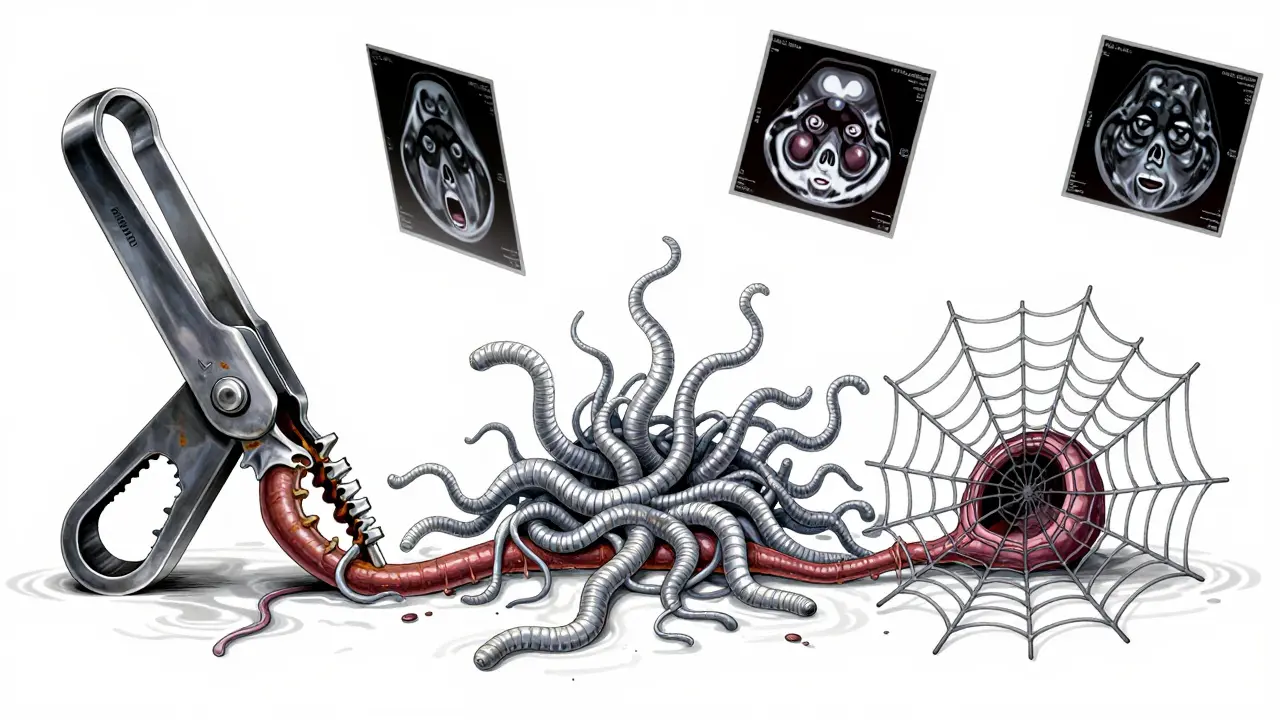
Treatment Options: Clipping, Coiling, or Flow Diversion
There are three main ways to treat an unruptured aneurysm-and each has trade-offs.
Surgical clipping is the oldest method. A neurosurgeon opens the skull, finds the aneurysm, and clamps it shut with a tiny titanium clip. It’s a direct fix. Success rates are high: 95% of aneurysms are fully blocked. Long-term, 88-92% stay sealed forever. But it’s invasive. Recovery takes weeks. Complications like stroke or infection happen in about 5% of cases.
Endovascular coiling is less invasive. A catheter is threaded from the groin up to the brain. Tiny platinum coils are pushed into the aneurysm, causing a clot to form inside. No skull opening. Most patients go home in a day or two. But it’s not always permanent. About 16% of coiled aneurysms need a second procedure within 12 years. Still, the 1-year death rate is lower than with clipping-8.1% versus 10.1%.
Flow diversion is the newest option. A mesh stent called a Pipeline Embolization Device is placed across the aneurysm neck. Blood flows through the stent, bypassing the bulge. Over months, the aneurysm slowly shrinks and seals off. It’s ideal for wide-necked or large aneurysms that can’t be coiled. Success rates hit 85% at one year. But it requires long-term anti-clotting meds, and there’s a small risk of delayed stroke.
For aneurysms at the base of the brain-like those in the middle cerebral artery-clipping is often preferred. For posterior circulation aneurysms, coiling or flow diversion are safer because the surgery is riskier. Age matters too. Patients over 70 have a 35% higher chance of complications with open surgery.
The New Kids on the Block: WEB and Beyond
There’s a new device called the WEB (Woven EndoBridge), approved in 2019. It’s like a tiny mesh ball placed inside a wide-necked aneurysm at a branch point in the artery. In trials, 71% were fully closed after one year. It’s especially helpful for aneurysms that are too wide for traditional coiling.
And research is moving fast. Scientists are now using machine learning to predict rupture risk by analyzing over 40 features-size, shape, location, blood flow patterns, even genetic markers. The HUNT study found 17 gene variants linked to aneurysm formation. In the future, a simple blood test might tell you your risk before an aneurysm even forms.
What If You Don’t Treat It?
Many small, low-risk aneurysms are left alone. The UCAS Japan study showed that aneurysms under 5 mm in the front of the brain have only a 0.2% chance of rupturing over five years. In the back of the brain, it’s 0.7%. That’s lower than the risk of a car accident on your daily commute.
Monitoring with annual MRA scans is safe and effective. If the aneurysm grows-even by 1 mm-that’s a signal to act. Growth is the strongest predictor of rupture. That’s why doctors don’t just look at size at diagnosis-they track changes over time.
Living with an Aneurysm: What You Can Do Today
Even if you’re not getting surgery, you can lower your risk right now:
- Get your blood pressure under 130/80. Medications like ACE inhibitors help-but lifestyle matters more. Walk daily. Cut salt. Lose weight if needed.
- Quit smoking. No exceptions. Even vaping raises risk. Talk to your doctor about nicotine replacement or prescription aids.
- Limit alcohol. Stick to under 14 drinks a week. One drink a day is fine. More than that? It’s adding pressure to a weak spot.
- Avoid heavy lifting and intense straining. That sudden spike in blood pressure can trigger rupture.
- Manage stress. Chronic stress raises blood pressure and inflammation. Meditation, sleep, and regular exercise help more than you think.
And if you’ve been told you have an unruptured aneurysm? Don’t panic. Most people live full lives without ever having a problem. But don’t ignore it either. Follow your doctor’s plan. Get your scans. Control your habits. Your brain will thank you.
What Happens After Treatment?
Success isn’t just about closing the aneurysm-it’s about staying closed. After clipping, you’ll need a follow-up angiogram in 6-12 months to confirm the clip is holding. After coiling or flow diversion, you’ll need MRA scans every 6-12 months for several years. Some aneurysms slowly reopen. That’s why monitoring doesn’t stop after treatment.
Quality of life is better with less invasive methods. People who had coiling or flow diversion report higher energy levels and better mobility at one year than those who had surgery. EQ-5D scores (a standard quality-of-life measure) were 0.82 for endovascular patients versus 0.76 for surgical patients.
And the long-term payoff? Successful treatment cuts your 10-year re-rupture risk from 68% down to just 2.3%. That’s the difference between living in fear and living freely.
Can a cerebral aneurysm go away on its own?
No, a cerebral aneurysm won’t disappear without treatment. It may stay stable for years, but it doesn’t heal. The weakened vessel wall remains vulnerable. Some small aneurysms grow very slowly and may never rupture, but they don’t shrink or vanish on their own. Monitoring is essential because growth is the biggest warning sign.
Is a cerebral aneurysm hereditary?
Yes, in some cases. If two or more close family members-like parents, siblings, or children-have had a brain aneurysm, your risk increases fourfold. Certain genetic conditions like polycystic kidney disease, Ehlers-Danlos syndrome, or Marfan syndrome also raise the risk. If you have a family history, talk to your doctor about screening, especially after age 30.
What are the warning signs of a ruptured aneurysm?
A ruptured aneurysm causes a sudden, severe headache-often described as the "worst headache of your life." Other signs include nausea, vomiting, stiff neck, blurred vision, sensitivity to light, seizures, or loss of consciousness. These symptoms come on instantly. If you or someone else experiences this, call emergency services immediately. Every minute counts.
Can you live a normal life with an unruptured aneurysm?
Absolutely. Many people live for decades with an unruptured aneurysm without any symptoms. The key is managing risk factors: controlling blood pressure, quitting smoking, avoiding heavy lifting, and following your doctor’s monitoring plan. Most people can work, exercise, travel, and enjoy life normally-just with a few lifestyle adjustments.
How often should you get scanned if you have an unruptured aneurysm?
Annual MRA scans are standard for unruptured aneurysms that are being monitored. If the aneurysm is small and low-risk, scans may be spaced out to every 2-3 years after a few stable years. But if it grows, changes shape, or your PHASES score increases, scans become more frequent. Always follow your neurologist’s recommendation-timing depends on your individual risk profile.
Are there any natural remedies or supplements that help prevent rupture?
No supplement or natural remedy has been proven to reduce aneurysm rupture risk. While antioxidants and anti-inflammatory diets are healthy, they don’t replace medical management. The only proven ways are controlling blood pressure, quitting smoking, and avoiding alcohol excess. Be wary of claims online-some supplements can even raise blood pressure or interfere with medications. Always check with your doctor before taking anything new.
What’s Next?
If you’ve been diagnosed with an unruptured aneurysm, your next step isn’t panic-it’s planning. Ask your doctor: What’s my PHASES score? Is my aneurysm growing? What are the pros and cons of each treatment option for my case? Get a second opinion if you’re unsure. Don’t rush, but don’t delay. The goal isn’t to eliminate all risk-it’s to reduce it to a level where you can live without fear.
And if you haven’t been diagnosed but have a family history or high blood pressure? Talk to your doctor about screening. A simple MRA can give you peace of mind-or the chance to act before it’s too late.


Jane Lucas
December 27, 2025 AT 12:04i had no idea aneurysms could be this silent. my aunt had one and we thought it was just a bad migraine. thanks for laying this out so clearly.
Kylie Robson
December 27, 2025 AT 16:19From a neurovascular imaging perspective, the hemodynamic parameters-particularly oscillatory shear stress (OSS) and wall shear stress (WSS) gradients-are critical biomarkers for rupture potential. The PHASES score, while clinically pragmatic, lacks granular fluid-structure interaction data that high-resolution 4D flow MRI can now capture. We’re entering an era where computational fluid dynamics (CFD) models predict rupture risk with >90% sensitivity in prospective cohorts.
Olivia Goolsby
December 27, 2025 AT 18:23Of course they’re pushing these treatments-medical device companies make billions off coiling and flow diverters. Did you know the Pipeline device was approved on a 12-month trial with only 147 patients? And they don’t tell you that 1 in 5 patients on antiplatelets after flow diversion end up with GI bleeds or intracranial hemorrhages from over-anticoagulation. Big Pharma doesn’t want you to know that watchful waiting might be safer… for them.
Will Neitzer
December 29, 2025 AT 02:29This is one of the most thorough, clinically accurate summaries I’ve seen on this topic. The distinction between size, shape, and hemodynamic stress is critical-and too often oversimplified in patient materials. I’ve shared this with my neurology residents. The PHASES score explanation is particularly well-articulated. Thank you for grounding this in evidence, not fear.
Miriam Piro
December 29, 2025 AT 09:29They say smoking triples your risk… but have you ever wondered who really profits from that stat? Tobacco companies fund half the studies on vascular disease. And who owns the MRI machines? Who profits when you get a "routine scan"? I’ve got a 3mm aneurysm and I’m not touching a scalpel or a coil-my body’s been through enough. The system wants you scared, medicated, and dependent. Wake up.
Also, did you know the FDA approved WEB after a trial where 3 patients died and 12 had strokes? But the press release said "90% success rate"… because they counted "partial occlusion" as success. 😒
Todd Scott
December 29, 2025 AT 18:44As someone who’s worked in neurosurgery for 22 years across three continents, I’ve seen everything from rural clinics in Nigeria to Ivy League hospitals. The truth? In low-resource settings, the biggest killer isn’t the aneurysm-it’s the lack of access to MRA or even basic neurology care. In rural Nigeria, patients present with ruptured aneurysms because screening is a luxury. This article is fantastic for those with access-but let’s not pretend equity exists. We need global screening protocols, not just fancy algorithms.
Also, yes-vaping raises risk. The nicotine-induced endothelial dysfunction is identical to cigarette smoke. And no, CBD oil won’t help. Don’t fall for TikTok "natural cures."
Chris Garcia
December 30, 2025 AT 11:24From Lagos to Los Angeles, the story is the same: our bodies are under siege by modern life. High blood pressure isn’t just a number-it’s the sound of stress, of processed food, of sleepless nights, of chasing money instead of peace. An aneurysm is not a glitch in your biology-it’s a scream from your soul. You can’t coil away trauma. You can’t clip away systemic neglect. But you can choose to walk. To breathe. To eat real food. To rest. The body knows how to heal-if we stop interfering with fear and start listening with humility.
Nikki Thames
December 30, 2025 AT 15:18I find it deeply concerning that this article normalizes the idea that "watchful waiting" is acceptable. When you have an unruptured aneurysm, you are not "living normally." You are living under a ticking clock that no one else can see. The psychological burden is immense. And yet, society tells you to "just manage your blood pressure" as if that’s a cure. It’s not. It’s a temporary bandage on a wound that could explode at any moment. This isn’t empowerment-it’s gaslighting disguised as medical advice.
Janice Holmes
January 1, 2026 AT 00:18FLOW DIVERSION?! Oh honey. That’s just a fancy stent with a 17% rebleed rate at 5 years. And don’t get me started on the antiplatelet regimen-your platelets are basically on life support. I had a friend who had a flow diverter and ended up with a subarachnoid hemorrhage 14 months later because she skipped her aspirin for a weekend trip. And they call that "minimally invasive"? It’s a Trojan horse wrapped in a mesh stent. 😭
Andrew Gurung
January 2, 2026 AT 13:05Let’s be real-this article is just a 10,000-word ad for neurointerventional radiology. Who’s paying for these studies? Who owns the patents on the WEB device? Who profits when you get a "routine MRA" every year? It’s not about health. It’s about revenue streams. And if you’re not getting treated? You’re just a statistic waiting to be monetized. 🤡
Also, I’ve read the HUNT study. Those "17 gene variants"? Most are SNPs with odds ratios under 1.2. That’s not science-that’s data dredging with a fancy name. Wake up.
John Barron
January 4, 2026 AT 08:58As a neurologist who’s reviewed 1,200+ aneurysm cases, I can confirm: the PHASES score is the most validated tool we have-but it’s still probabilistic, not deterministic. The biggest mistake patients make? Treating the score like a death sentence. A PHASES of 6 doesn’t mean "you’re going to die." It means "you have a 12% chance of rupture in 5 years." That’s less than the risk of dying in a car crash during a 100-mile drive. But it’s also not "ignore it." It’s a call to action: control BP, quit smoking, get scans. Not panic. Not surgery. Action. And if you’re over 70? Coiling is almost always the right choice. Clipping is for the young, the healthy, and the brave.
Nicola George
January 4, 2026 AT 15:36so i had a 4mm aneurysm in my ACoA. doctor said "watch and wait." i quit smoking, started walking 5 miles a day, and stopped eating anything with a label. 3 years later, scan showed it shrank by 0.5mm. not magic. just biology. your body wants to live. stop feeding it poison.
James Bowers
January 6, 2026 AT 12:57The notion that "some aneurysms never rupture" is dangerously misleading. The UCAS Japan study has significant selection bias-patients were screened only if they presented with symptoms or had family history. Asymptomatic populations are not represented. Furthermore, the 0.2% annual rupture rate for small anterior aneurysms is derived from a cohort with an average age of 58. Extrapolating this to younger patients is statistically invalid. The data does not support complacency. Monitoring is not passive-it is active surveillance requiring rigorous protocol adherence. Failure to comply constitutes medical negligence.