Antibiotic Selection Tool
Select Your Clinical Scenario
Recommended Options
Key Takeaways
- Cefixime is a third‑generation cephalosporin with strong activity against many Gram‑negative infections.
- Amoxicillin, azithromycin, ciprofloxacin, doxycycline and levofloxacin cover overlapping but distinct bacterial spectra.
- Choosing the right drug depends on infection type, local resistance patterns, patient allergies and side‑effect tolerance.
- All antibiotics share common risks: GI upset, allergic reactions and potential drug interactions.
- Consult a healthcare professional before switching antibiotics; self‑medication can fuel resistance.
When a doctor prescribes an oral antibiotic, patients often wonder whether there’s a better option. Cefixime comparison is a frequent search because the drug sits somewhere between broad‑spectrum penicillins and fluoroquinolones. Below you’ll get a clear, side‑by‑side look at Cefixime and the most common alternatives, so you can understand when each one makes sense.
What is Cefixime?
Cefixime is a third‑generation cephalosporin antibiotic that works by inhibiting bacterial cell‑wall synthesis. First approved in the early 1990s, it is taken orally and is stable against many beta‑lactamases, giving it an edge over older penicillins in resistant infections.
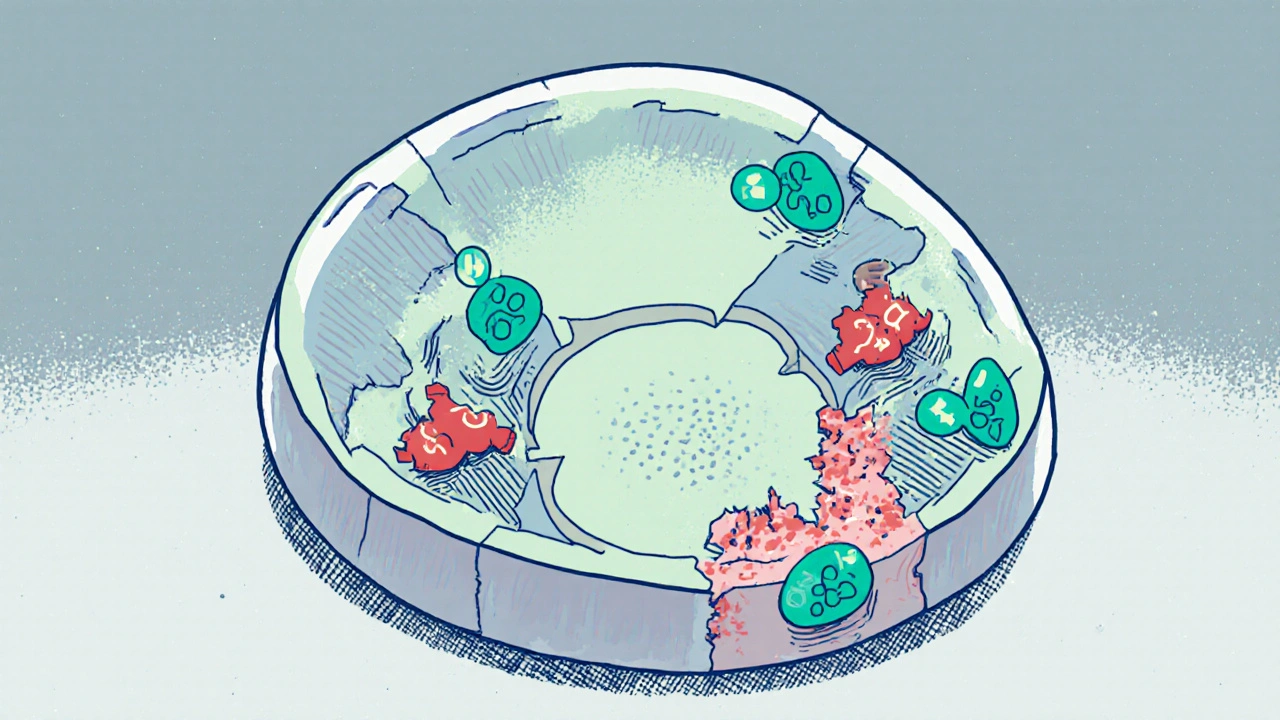
How Cefixime Works
Cefixime targets the penicillin‑binding proteins (PBPs) that build bacterial cell walls. By binding to these proteins, it prevents cross‑linking of peptidoglycan strands, causing the wall to weaken and the cell to burst. This mechanism is especially effective against Gram‑negative organisms such as Escherichia coli and Klebsiella pneumoniae, which are common culprits in urinary‑tract and gastrointestinal infections.
Common Alternatives at a Glance
Below are the most frequently prescribed oral antibiotics that patients compare with Cefixime.
- Amoxicillin - a broad‑spectrum penicillin, excellent for many Gram‑positive and some Gram‑negative infections.
- Azithromycin - a macrolide that concentrates in tissues and is often used for respiratory infections.
- Ciprofloxacin - a fluoroquinolone with strong activity against Gram‑negative bacteria, especially in urinary‑tract infections.
- Doxycycline - a tetracycline useful for atypical pathogens and tick‑borne diseases.
- Levofloxacin - a newer fluoroquinolone offering a broader spectrum than ciprofloxacin but with similar safety concerns.
Side‑Effect Profiles
All antibiotics carry a risk of adverse events. Here’s a quick look at the most common complaints.
| Antibiotic | GI upset | Allergic reaction | Specific concerns |
|---|---|---|---|
| Cefixime | Moderate | Rare, cross‑reactivity with penicillins ~1% | May cause biliary sludge in high‑dose therapy |
| Amoxicillin | Low‑to‑moderate | Common (rash, hives) | Risk of Clostridioides difficile colitis |
| Azithromycin | Low | Moderate (esp. in asthma) | QT‑prolongation in high doses |
| Ciprofloxacin | Low‑moderate | Rare | Tendinitis, peripheral neuropathy, cartilage damage (caution in young) |
| Doxycycline | Low‑moderate | Rare | Photosensitivity, esophageal irritation |
| Levofloxacin | Low‑moderate | Rare | Similar to ciprofloxacin plus risk of severe tendon rupture |
When to Choose Cefixime Over Others
- Suspected Gram‑negative urinary‑tract infection where local resistance data show >20% resistance to trimethoprim‑sulfamethoxazole.
- Patients with penicillin allergy but who need a beta‑lactam effect; cefixime's cross‑reactivity is low.
- Need for once‑daily dosing - Cefixime’s 200mg tablet maintains therapeutic levels for 24hours, improving adherence.

When Alternatives May Be Better
- Respiratory infections caused by atypical bacteria (Mycoplasma, Chlamydia) - azithromycin or doxycycline cover these better.
- Severe skin or soft‑tissue infections - clindamycin or a fluoroquinolone like levofloxacin may provide broader anaerobic coverage.
- High local resistance to cephalosporins - amoxicillin‑clavulanate or a fluoroquinolone can bypass beta‑lactamase mediated resistance.
Practical Checklist for Selecting an Antibiotic
Before you or your clinician settles on a drug, run through this short list.
- Identify the likely pathogen (Gram‑positive, Gram‑negative, atypical).
- Check local antibiogram data for resistance rates.
- Confirm any known drug allergies (especially penicillin or sulfa).
- Consider patient factors: age, pregnancy status, kidney function.
- Review potential drug-drug interactions (e.g., macrolides with statins).
- Assess dosing convenience - once daily vs multiple doses.
Frequently Asked Questions
Is Cefixime effective for sinus infections?
Cefixime can treat sinusitis caused by susceptible Gram‑negative bacteria, but it lacks strong activity against common Streptococcus pneumoniae strains. For uncomplicated sinusitis, a macrolide (azithromycin) or amoxicillin‑clavulanate is usually preferred.
Can I take Cefixime if I’m pregnant?
Cefixime is classified as Pregnancy Category B in Australia, meaning animal studies have shown no risk and there are no controlled human studies. It is generally considered safe, but a doctor should weigh benefits against any potential risk.
How does the cost of Cefixime compare to amoxicillin?
In 2025 Australian retail pricing, a standard 7‑day course of 200mg Cefixime tablets costs about AUD 30-35, while a 7‑day supply of amoxicillin 500mg capsules is roughly AUD 12-15. Insurance coverage can narrow the gap, but amoxicillin remains the cheaper option for most patients.
What should I do if I miss a dose of Cefixime?
Take the missed dose as soon as you remember, unless it’s less than 12hours until the next scheduled dose. In that case, skip the missed pill and continue with the regular schedule. Do not double‑dose.
Are there any foods I should avoid while on Cefixime?
Cefixime absorption isn’t significantly affected by food, but taking it with a full glass of water helps prevent esophageal irritation. Dairy products don’t interfere, unlike some tetracyclines.
Bottom line: Cefixime shines when you need a reliable, once‑daily, Gram‑negative‑focused oral agent and you have a mild penicillin allergy. For broader coverage, different pathogen types, or cost‑sensitive situations, the alternatives listed above often make more sense. Always let a healthcare professional tailor the choice to your specific infection and health profile.


jake cole
October 14, 2025 AT 15:05Cefixime is overpriced nonsense and you might as well waste your cash on cheaper amoxicillin. The once‑daily gimmick doesn’t justify the inflated price tag.
Natalie Goldswain
October 15, 2025 AT 13:18i think that cost part matters a lot lol.
Melissa Trebouhansingh
October 16, 2025 AT 11:31One must begin by acknowledging the nuanced interplay of pharmacodynamics and patient compliance without resorting to mere superficial comparisons. Cefixime, as a third generation cephalosporin, offers a spectrum that intersects yet diverges from both penicillins and fluoroquinolones. Its pharmacokinetic profile allows for a once daily regimen which inherently promotes adherence especially in populations prone to missed doses. However, the assertion that it is universally superior neglects the pivotal role of local resistance patterns which can dramatically alter therapeutic outcomes. In regions where beta‑lactamase production is rampant, the purported advantage of cefixime may be nullified. Moreover, the cost differential, while notable, must be contextualized within the broader healthcare economics which include generic availability and insurance formularies. The safety profile, though generally favorable, is not devoid of concerns such as biliary sludge formation at high dosages. Comparative efficacy against common uropathogens remains contingent on susceptibility data, a factor often overlooked in blanket recommendations. Patients with documented penicillin allergy may indeed benefit from the low cross‑reactivity of cefixime, yet this is not an exclusive indication. Respiratory indications, where azithromycin or amoxicillin‑clavulanate excel, do not align with cefixime’s optimal use cases. The once daily dosing, while convenient, does not compensate for suboptimal tissue penetration in certain infections. In dermatologic applications, agents with superior anaerobic coverage may be preferred. The conversation must also incorporate patient-specific variables such as renal function which influence dose adjustments. Ultimately, the decision matrix is multidimensional and resists reduction to a simplistic hierarchy.
maurice screti
October 17, 2025 AT 09:45Honestly the whole thing feels like a marketing fluff fest-yeah, once‑daily is cool, but if you’ve got a stubborn infection, you’ll still need something with a broader shield. I’d say look at the local antibiogram before you start throwing cefixime at everything.
Abigail Adams
October 18, 2025 AT 07:58From a clinical standpoint, it is imperative to recognize that the selection of an antibiotic cannot be predicated solely on dosing convenience. The pharmacologic attributes of cefixime, while commendable in certain Gram‑negative urinary isolates, fall short when confronting atypical pathogens which necessitate macrolide or tetracycline therapy. Moreover, the potential for adverse events such as biliary sludge, albeit infrequent, warrants vigilant monitoring. In light of these considerations, the recommendation of cefixime as a first‑line agent should be confined to well‑defined scenarios supported by susceptibility data.
Belle Koschier
October 19, 2025 AT 06:11I hear you, but let’s keep it balanced-cefixime can be a good choice for uncomplicated UTIs when resistance is low, yet it’s not a catch‑all. Always weigh allergy history and pregnancy status before deciding.
Allison Song
October 20, 2025 AT 04:25One might contemplate the broader philosophical implication of antimicrobial stewardship: each prescription is an ethical decision that reverberates through microbial ecosystems. Choosing cefixime wisely aligns with the principle of minimal harm.
Joseph Bowman
October 21, 2025 AT 02:38Hey folks, ever wonder why the pharma giants push these “once‑daily” pills? Looks like a way to keep us hooked without noticing the deeper agenda. They say it’s about compliance, but maybe it’s about data collection on who’s taking what and when.
Singh Bhinder
October 22, 2025 AT 00:51Curious if anyone has seen recent local resistance stats for cefixime in the Midwest? It’d help to know if it’s still a solid pick for uncomplicated UTIs or if we should pivot to amox.
Kelly Diglio
October 22, 2025 AT 23:05Thank you for sharing this thorough comparison. It is reassuring to see the emphasis on individualized care and the cautious approach to pregnancy categories. This will definitely guide my next discussion with the clinician.
Carmelita Smith
October 23, 2025 AT 21:18Great summary! 😊
Liam Davis
October 24, 2025 AT 19:31Here’s a quick cheat‑sheet for clinicians:
• Cefixime – Best for Gram‑negative UTIs, once‑daily dosing, Category B in pregnancy.
• Amoxicillin – Cost‑effective, excellent for Gram‑positive infections, Category B.
• Azithromycin – Ideal for atypical respiratory pathogens, macrolide class, QT‑monitoring needed.
• Ciprofloxacin – Potent against Gram‑negative urinary and GI infections, beware of tendon‑related adverse events, Category D in pregnancy.
• Doxycycline – Great for tick‑borne diseases, photosensitivity, Category D.
• Levofloxacin – Broad spectrum, similar tendon risks as ciprofloxacin, Category D.
When prescribing, always cross‑check local antibiograms, patient allergies, and renal function. And remember: adherence improves with simpler dosing, but not at the expense of efficacy.
Arlene January
October 25, 2025 AT 17:45Awesome breakdown! Let’s keep the conversation positive and help each other pick the right drug for the right case. You’ve got this!
Kaitlyn Duran
October 26, 2025 AT 14:58Is there any info on how cefixime performs in kids? I’m trying to understand pediatric dosing.
Terri DeLuca-MacMahon
October 27, 2025 AT 13:11Wow, such a helpful post! 🎉👍 Let’s spread the word and make sure everyone gets the right information – it’s all about good health, after all! 🌟