What You Need to Know Before Choosing Between Gastric Bypass and Sleeve Gastrectomy
If you’re considering bariatric surgery, you’ve probably heard about two main options: gastric bypass and sleeve gastrectomy. Both are proven ways to lose weight when diet and exercise haven’t worked. But they’re not the same. One changes how your body absorbs food. The other just makes your stomach smaller. The choice isn’t just about which one loses more weight-it’s about which one fits your life, health, and long-term goals.
In 2022, over 286,000 bariatric surgeries were done in the U.S. Sixty-three percent of them were sleeve gastrectomies. Only 27% were gastric bypasses. That’s a big shift from 15 years ago, when bypass was the go-to. So why did the numbers flip? And which one should you pick?
How Each Procedure Works
Gastric bypass, or Roux-en-Y gastric bypass, is more complex. Surgeons create a tiny stomach pouch-about the size of a golf ball-and connect it directly to the middle part of your small intestine. That skips most of your stomach and the first section of your intestine. Food doesn’t go through the usual digestive path. That means fewer calories get absorbed. It’s not just about eating less-it’s about your body absorbing less.
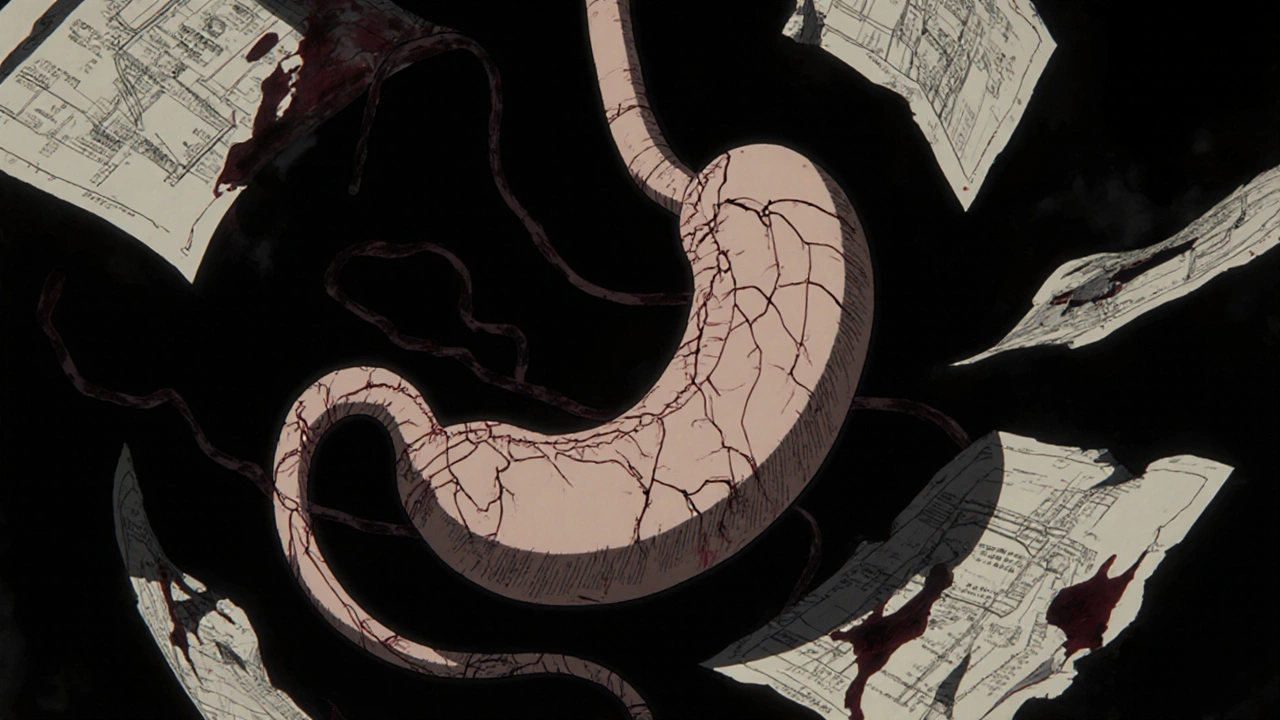
Sleeve gastrectomy is simpler. About 80% of your stomach is removed, leaving a narrow tube shaped like a banana. That’s it. No rerouting. No bypassing. Just a smaller stomach that fills up faster and sends fewer hunger signals to your brain. The surgery takes less time-around 47 minutes on average, compared to 68 for bypass.
Both are done laparoscopically, meaning small cuts, less pain, and faster healing. Most people leave the hospital in just one day.
Weight Loss Results: Which One Works Better?
When it comes to losing weight, gastric bypass usually wins-by a little.
At the five-year mark, people who had gastric bypass lost about 57% of their excess body weight. Those who had sleeve gastrectomy lost around 49%. That’s a real difference, but not huge. Some people lose more, some less. It depends on how well you stick to your diet and exercise plan after surgery.
UPMC data shows gastric bypass patients often lose 60-80% of excess weight within 12 to 18 months. Sleeve patients typically lose 60-70% over the same time-but it tends to happen more slowly. The University of Rochester says bypass may lead to faster, greater weight loss. But sleeve still delivers life-changing results.
And here’s something important: long-term, people who had bypass are less likely to regain weight. Studies show sleeve patients are more likely to need a second surgery later on. About 5% of sleeve patients end up needing revision surgery within five years, compared to just 1.8% for bypass.

Risks and Complications: Safety Matters
More weight loss doesn’t always mean better outcomes. Safety is just as important.
A 2022 study of nearly 96,000 Medicare patients found that sleeve gastrectomy had a lower risk of death within five years: 4.27% for sleeve vs. 5.67% for bypass. That’s a 33% lower risk of dying after surgery.
Complications like infections, leaks, or blood clots are also less common with sleeve. But bypass has its own risks: vitamin and mineral deficiencies. Because food skips parts of the intestine, your body can’t absorb enough iron, calcium, vitamin B12, or folate. That means lifelong supplements-and regular blood tests every six months.
Sleeve patients usually only need one blood test a year. They’re less likely to have nutrient problems. But they’re more likely to get acid reflux after surgery. About 15-20% of sleeve patients develop new or worse GERD. Gastric bypass, on the other hand, often improves reflux.
Then there’s dumping syndrome. It happens in 50-70% of bypass patients. Eat something sugary or fatty, and you might get nausea, sweating, dizziness, or diarrhea within 30 minutes. It’s unpleasant-but it also keeps you from eating junk food. Many people say it’s the best “enforcement tool” they never knew they needed.
Metabolic Benefits: Diabetes, Blood Pressure, and More
If you have type 2 diabetes, high blood pressure, or sleep apnea, bariatric surgery can reverse or improve those conditions. But which surgery does it better?
Gastric bypass tends to win here, too. Studies show it leads to higher rates of diabetes remission. One reason? The rerouting of food changes gut hormones that control blood sugar. Dr. Amir Ghaferi from Michigan Medicine says the malabsorptive part of bypass helps insulin work better.
That’s why some doctors still recommend bypass for patients with severe diabetes-even if they’re not the heaviest. The JAMA Network Open study found hypertension improved more often in bypass patients. Sleep apnea improved in both, but slightly more with bypass.
Still, sleeve gastrectomy helps too. Most people see their blood pressure drop within months. Many stop taking diabetes meds within a year. The difference isn’t night and day-but it’s there.
Recovery and Lifestyle Changes
Recovery time is similar: 2-4 weeks before returning to normal activities. But the daily life changes are very different.
Sleeve patients often say their recovery feels easier. No dumping syndrome. Fewer supplements. Less strict diet rules early on. But many report feeling hungrier longer-term. The stomach is smaller, but not as altered hormonally. Cravings can return.
Gastric bypass patients often say they feel full faster and stay full longer. Hunger drops dramatically. But they have to be much more careful. No soda. No candy. No fried food. Even small mistakes trigger dumping. Many say it’s a constant reminder to eat clean.
On Reddit’s r/bariatrics, one patient wrote: “I had the sleeve. I lost 120 pounds. But I still snack. I still get hungry. I wish I’d known how much harder it is to stay full.” Another said: “Bypass was brutal at first. But now? I don’t even think about food the way I used to.”

Cost and Insurance: What You’ll Pay
Insurance usually covers both procedures if you have a BMI over 40-or over 35 with conditions like diabetes or high blood pressure. But some insurers, like UnitedHealthcare, now require a BMI of 45 or higher as of early 2024.
Out-of-pocket costs vary. On average, sleeve gastrectomy costs about $14,500 after insurance pays its share. Gastric bypass runs closer to $19,300. That’s a $4,800 difference. Why? Bypass is longer, more complex, and requires more follow-up care.
But here’s the catch: if you need revision surgery later because of weight regain or complications, that’s not always covered. And revision surgery after a sleeve can cost even more than the original bypass.
Which One Should You Choose?
There’s no one-size-fits-all answer. But here’s how to think about it:
- Choose gastric bypass if: You have type 2 diabetes, severe GERD, or need the strongest chance of lasting weight loss. You’re willing to take lifelong supplements and avoid sugar completely. You want the lowest chance of needing another surgery.
- Choose sleeve gastrectomy if: You want a simpler surgery with fewer complications, fewer supplements, and faster recovery. You’re okay with a slightly slower weight loss and higher chance of needing revision later. You’re not diabetic or don’t have severe reflux.
Most people who choose sleeve do so because it feels safer and easier. But many who choose bypass say it changed their life more deeply.
What’s Next for Bariatric Surgery?
Surgeons are now experimenting with hybrid procedures-like a “mini-bypass” or a sleeve with a small bypass section. The goal? Get the benefits of both without the worst risks.
Also, new endoscopic techniques are being tested to fix weight regain after sleeve surgery-without another major operation. These aren’t standard yet, but they’re coming.
Right now, the data is clear: sleeve is more popular. But bypass still delivers more long-term results for many. The best choice isn’t about what’s trending. It’s about what matches your health, habits, and goals.
Which surgery leads to more weight loss: gastric bypass or sleeve gastrectomy?
Gastric bypass typically leads to more weight loss. At the five-year mark, patients lose about 57% of excess weight with bypass versus 49% with sleeve. Gastric bypass also has a lower rate of weight regain over time, making it more effective for long-term results.
Is sleeve gastrectomy safer than gastric bypass?
Yes, sleeve gastrectomy is generally safer in the short and medium term. A 2022 study of nearly 96,000 patients found a 33% lower risk of death within five years compared to gastric bypass. Sleeve also has fewer complications like nutrient deficiencies and internal hernias. However, it carries a higher risk of needing a revision surgery later.
Do I have to take vitamins for life after bariatric surgery?
Yes, but the requirement differs. After gastric bypass, you’ll need lifelong supplements for iron, calcium, vitamin B12, and folate, with blood tests every six months. After sleeve gastrectomy, you’ll still need supplements, but usually just once a year for monitoring. The risk of deficiency is much lower with sleeve.
Can bariatric surgery cure type 2 diabetes?
Yes, both surgeries can lead to remission of type 2 diabetes, but gastric bypass is more effective. Studies show 60-80% of bypass patients achieve remission within a year, compared to 50-70% for sleeve. The rerouting of the digestive tract in bypass improves insulin sensitivity more dramatically.
What is dumping syndrome, and does it happen with sleeve gastrectomy?
Dumping syndrome is a reaction to eating sugary or fatty foods too quickly after gastric bypass. Symptoms include nausea, sweating, dizziness, and diarrhea. It affects 50-70% of bypass patients and acts as a natural deterrent to unhealthy eating. It rarely occurs after sleeve gastrectomy because the digestive path isn’t altered.
Which surgery is cheaper: gastric bypass or sleeve gastrectomy?
Sleeve gastrectomy is typically about 25% cheaper. As of 2024, the average out-of-pocket cost for sleeve is $14,500, while gastric bypass is around $19,300. This is due to shorter surgery time, fewer complications, and less long-term monitoring needed.
Can I get pregnant after bariatric surgery?
Yes, but doctors recommend waiting 12-18 months after surgery to allow your body to stabilize and lose weight. Pregnancy after surgery is safer than during severe obesity. Both sleeve and bypass patients can have healthy pregnancies, but bypass patients need careful monitoring of nutrient levels to support fetal development.
Do I need to lose weight before surgery?
Most insurance companies require at least six months of documented weight management attempts before approving surgery. This includes seeing a dietitian, attending counseling, and trying non-surgical methods. It’s not about losing a certain amount-it’s about showing you’re ready to commit to lifelong changes.

Shivam Goel
November 22, 2025 AT 18:10Amy Hutchinson
November 24, 2025 AT 16:09Archana Jha
November 25, 2025 AT 23:41Aki Jones
November 27, 2025 AT 05:44Jefriady Dahri
November 28, 2025 AT 01:58Andrew McAfee
November 30, 2025 AT 00:11Elise Lakey
November 30, 2025 AT 03:44Roscoe Howard
November 30, 2025 AT 16:44Kimberley Chronicle
December 2, 2025 AT 05:29Karen Willie
December 3, 2025 AT 16:41