When a brand-name drug loses its patent, a cheaper version hits the market. That’s not just good news for patients-it’s a financial earthquake for the entire U.S. healthcare system. The FDA generic approvals don’t just make medicine more affordable-they save billions every single year. But how much? And does it really add up over time?
What the numbers actually show
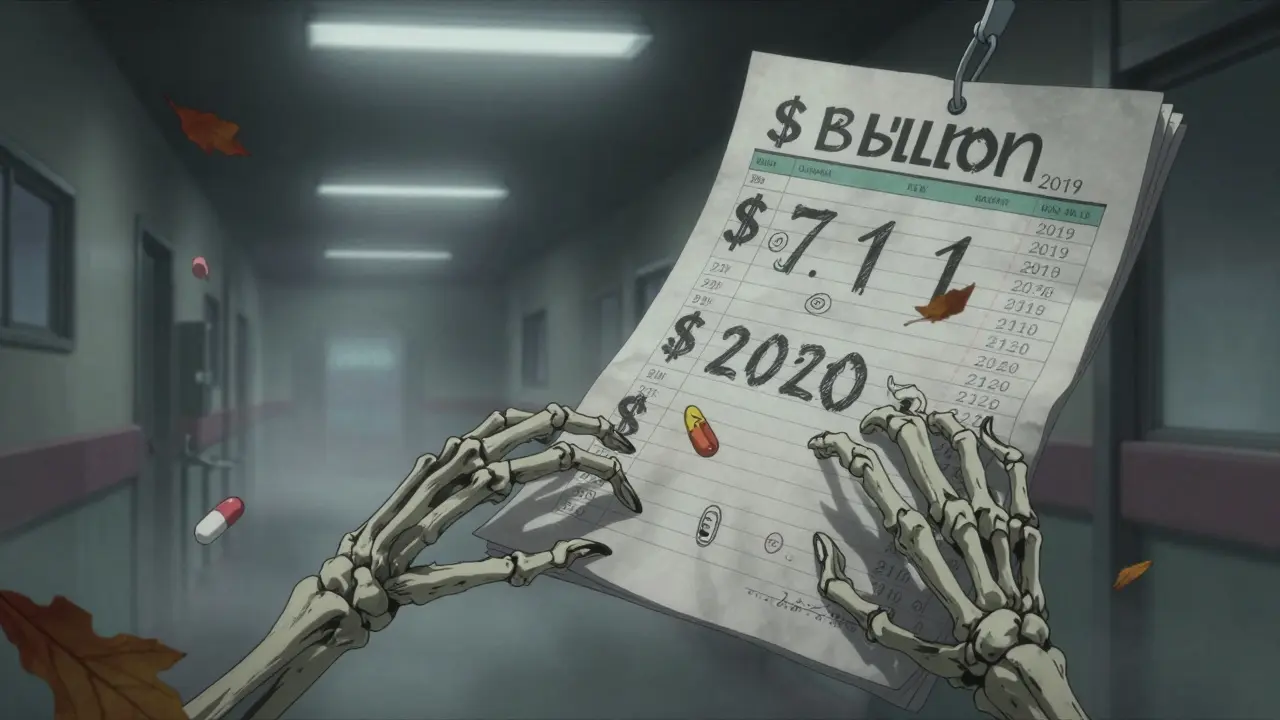
The FDA doesn’t just approve generic drugs. It tracks exactly how much money those approvals save. In 2019, a single wave of new generic approvals saved $7.1 billion in just 12 months. That’s more than the annual budget of many U.S. states. The next year? It dropped to $1.1 billion. Why? Because not every year has a blockbuster drug going generic. It’s not a steady stream-it’s a lottery. One year, you get a hit. The next, you get a handful of smaller drugs with modest savings. The 2022 numbers jumped again to $5.2 billion from first-time generic approvals alone. That spike came from a few big ones: drugs for high blood pressure, diabetes, and mental health. These aren’t niche meds. They’re taken by millions. When a $300-a-month brand-name pill drops to $15 as a generic, the savings ripple across insurers, pharmacies, and patients’ wallets.The bigger picture: total savings from all generics
But here’s where most people get confused. The $5.2 billion from new approvals in 2022 is just the tip of the iceberg. The real savings come from every generic drug already on the shelf, being filled every day. The Association for Accessible Medicines (AAM) tracks this. In 2023, generics saved the U.S. healthcare system $445 billion. That’s not a typo. Half a trillion dollars in one year. That’s because 90% of all prescriptions filled in the U.S. are generics. But they make up only 13% of total drug spending. That gap? That’s the savings. A patient on a $500 monthly brand-name drug might pay $10 for the generic. Multiply that by millions of prescriptions, and you get a number that dwarfs the annual savings from new approvals.Who benefits the most?
It’s not just patients. Medicare saved $137 billion in 2023 from generics. Commercial insurers saved $206 billion. Medicaid saved the rest. For a senior on fixed income, that $6.97 copay for a cholesterol med instead of $150 makes a real difference. For a family with a child on asthma inhalers, it’s the difference between filling the prescription or skipping it. California alone saved $38 billion in 2023. Alaska saved $354 million. It’s not about size-it’s about scale. Every state, every insurer, every pharmacy benefit manager feels the pinch when a brand drug goes generic. Even small towns see the effect: a local pharmacist might fill 50 generic prescriptions a day. At $20 each instead of $100, that’s $4,000 saved in one day.
Why the numbers jump around
The FDA’s yearly savings from new approvals fluctuate wildly. Why? Because it depends on what patents expire. In 2019, several high-revenue drugs lost protection at once. In 2020, fewer big ones did. That’s why 2019’s $7.1 billion looks like an outlier-it was. But the trend is clear: when a top-selling drug goes generic, the savings explode. Take 2021. Just five new generics accounted for half of the $1.7 billion saved from first-time approvals. One of them? A drug for Type 2 diabetes. Before the generic, it cost $500 a month. After? $30. That’s $470 saved per patient, per month. Multiply that by 2 million users? That’s nearly $12 billion in a single year.It’s not all smooth sailing
Here’s the catch: not all savings reach the patient. Pharmacy benefit managers (PBMs) negotiate rebates with drugmakers. A generic might cost $10, but the PBM takes $5 in rebates. The patient still pays $10. The savings are real, but they don’t always show up at the counter. A 2023 Senate investigation found only 50-70% of generic savings actually make it to consumers. Brand-name companies also delay generics with legal tricks-patent extensions, “pay-for-delay” deals, and complex REMS programs that block generic manufacturers from getting samples to test their products. The FDA’s 2023 Drug Competition Action Plan is trying to shut those down. But it’s an uphill battle.The future: biosimilars and complex drugs
Most of the savings so far come from small-molecule drugs-pills and capsules. But the next wave is coming from biosimilars: cheaper versions of complex biologic drugs used for cancer, rheumatoid arthritis, and Crohn’s disease. As of August 2024, the FDA had approved 59 biosimilars. They’re harder to make, harder to approve, and slower to catch on. But when they do, the savings are massive. One biosimilar for a cancer drug saved $15,000 per patient annually. Multiply that by thousands of patients? That’s billions. The FDA is also working on faster reviews for complex generics. Thanks to the GDUFA program, 95% of applications are reviewed in under 10 months. That means generics hit the market faster, and savings start sooner.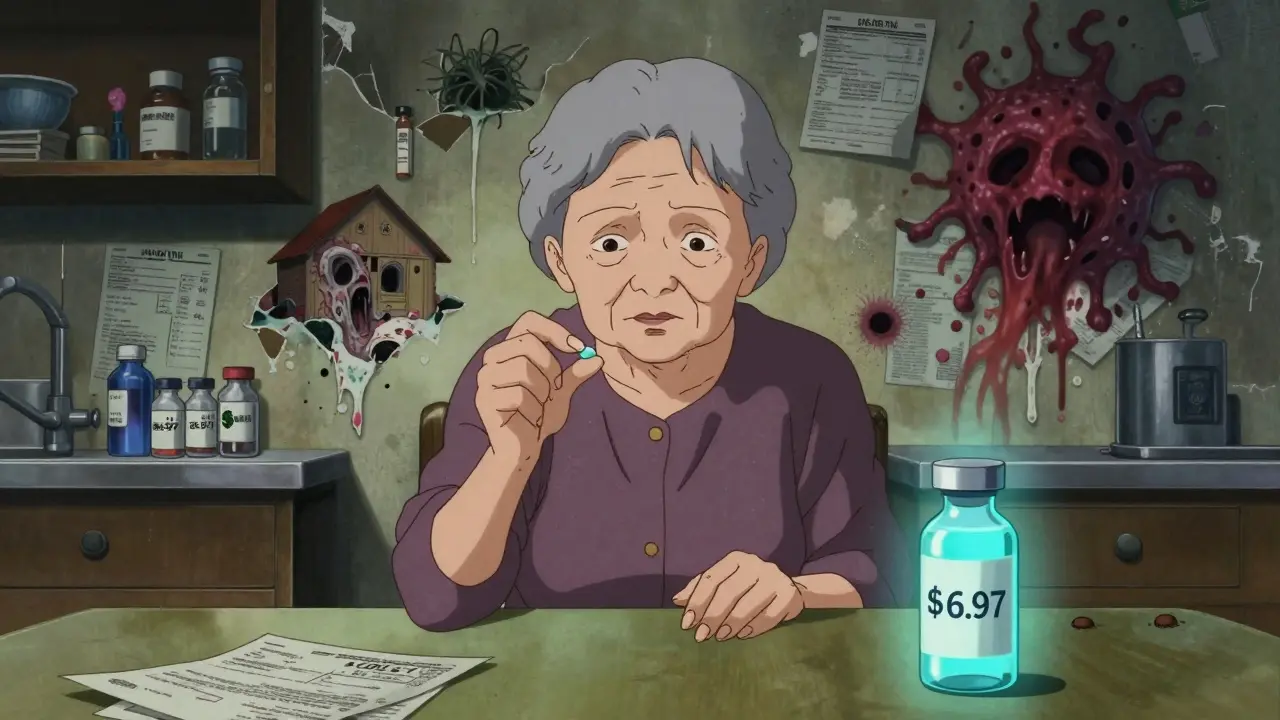
What this means for you
If you’re on a chronic medication, ask your pharmacist: Is there a generic? If you’re paying $100 for a pill that has a $15 generic version, you’re leaving money on the table. Even if your insurance covers it, you’re still paying more than you need to. Ask for the generic. Push back if your doctor says “it’s not the same.” It is. The FDA requires generics to be identical in active ingredient, strength, and effectiveness. If you’re an employer or a policy maker, the message is clear: supporting generic drug access isn’t just ethical-it’s economic. Every dollar saved on drugs is a dollar that can go to housing, food, or savings. And that’s not just good for individuals. It’s good for the whole system.Year-by-year savings: the real data
Here’s what the numbers look like for new generic approvals (FDA’s first-generic savings only):- 2018: $2.70 billion
- 2019: $7.10 billion
- 2020: $1.10 billion
- 2021: $1.37 billion
- 2022: $5.20 billion
- 2020: $338 billion
- 2022: $408 billion
- 2023: $445 billion
Why this matters beyond the numbers
It’s easy to treat these figures as abstract. But behind every billion saved is a person who didn’t have to choose between medicine and rent. A parent who could afford their child’s insulin. A veteran who didn’t skip their heart medication because the copay was too high. The FDA doesn’t just approve pills. It approves access. And every time a generic gets approved, it doesn’t just lower a price-it lowers a barrier. That’s the real value. Not just in dollars, but in lives.How much do generic drugs actually save patients per prescription?
On average, a generic drug costs 80-85% less than the brand-name version. For example, if a brand-name drug costs $150 a month, the generic might cost $20-$30. The average generic copay in 2019 was $6.97, compared to $78 for brand-name drugs. Many generics are available for under $10 at pharmacies like Walmart and Costco.
Why do some generic drugs cost more than others?
Price varies based on competition. If only one company makes the generic, it might cost more. But when five or six companies enter the market, prices drop sharply. Some drugs, especially older ones with no competition, can still be expensive. That’s why it’s worth checking prices at multiple pharmacies or using discount programs like GoodRx.
Do generics work as well as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also be bioequivalent-meaning they work the same way in the body. There’s no clinical difference in effectiveness or safety. The only differences are in inactive ingredients, like fillers or dyes, which don’t affect how the drug works.
Why don’t all drugs have generics?
Some drugs are still under patent protection. Others are too complex to copy easily-like biologics or injectables. Brand companies also use legal tactics to delay generics, such as filing patent lawsuits or creating restrictive access programs (REMS). The FDA is working to remove these barriers, but it takes time.
How do I find out if a generic is available for my medication?
Ask your pharmacist or doctor. You can also check the FDA’s Orange Book online, which lists approved generic equivalents. Many pharmacies will automatically substitute a generic unless your doctor writes "dispense as written" on the prescription. Always ask-don’t assume.
Are biosimilars the same as generics?
Not exactly. Generics are exact copies of small-molecule drugs. Biosimilars are highly similar versions of complex biological drugs, made from living cells. They’re not identical, but they’re proven to work the same way. Biosimilars are newer and cost less than the original biologic-often 15-35% cheaper-but they’re still more expensive than traditional generics.
Why do some insurance plans still prefer brand-name drugs?
Some plans have deals with drugmakers that pay them rebates if they push the brand-name version-even when a generic is available. This is called a rebate structure. It’s not always in the patient’s best interest. Always ask your insurer: "Is there a generic? What’s the copay?" You might be surprised how much you can save.
Can I switch to a generic without my doctor’s permission?
In most cases, yes. Pharmacists are allowed to substitute a generic unless the prescription says "dispense as written" or "no substitution." If your doctor hasn’t restricted substitution, your pharmacist can switch you to the generic without calling them. It’s legal, safe, and saves money.

Rachel Liew
February 1, 2026 AT 05:47Lisa Rodriguez
February 2, 2026 AT 14:57Ed Di Cristofaro
February 3, 2026 AT 19:25Angel Fitzpatrick
February 5, 2026 AT 17:16Donna Macaranas
February 6, 2026 AT 23:50Deep Rank
February 7, 2026 AT 12:35franklin hillary
February 9, 2026 AT 05:29Nidhi Rajpara
February 9, 2026 AT 05:50Sami Sahil
February 10, 2026 AT 03:51Ishmael brown
February 10, 2026 AT 18:15Jamie Allan Brown
February 11, 2026 AT 15:03Naomi Walsh
February 13, 2026 AT 06:52